P293 Correlation between clinical measures to capture disease burden and prediction of the initial course of Crohn’s disease - findings from a Copenhagen IBD Inception Cohort Study (IBD Prognosis Study)
Attauabi, M.(1,2)*;Madsen, G.R.(2,3);Bendtsen, F.(2,3);Bjerrum, J.T.(1);Wilkens, R.(4);Theede, K.(2,3);Ilvemark, J.F.K.F.(2,3);Boysen, T.(2,3);Seidelin, J.B.(1);Burisch, J.(2,3);
(1)Copenhagen University Hospital - Herlev and Gentofte, Department of Gastroenterology and Hepatology, Herlev, Denmark;(2)Hvidovre Hospital, Copenhagen Center for Inflammatory Bowel Disease in Children- Adolescents- and Adults, Hvidovre, Denmark;(3)Copenhagen University Hospital - Amager and Hvidovre, Gastrounit- Medical Section, Hvidovre, Denmark;(4)Copenhagen University Hospital - Bispebjerg and Frederiksberg, Digestive Disease Center, Copenhagen, Denmark;
Background
The initial disease burden of Crohn’s disease (CD) is dissimilar across patients; however, the ability to capture and predict the disease burden at diagnosis is scarcely investigated. The aim of the current study was to describe the initial disease burden of Crohn’s disease.
Methods
IBD Prognosis Study is an ongoing prospective population-based inception cohort of newly diagnosed patients with CD between May 1st, 2021, and November 1st, 2022, according to the Copenhagen IBD Criteria.1 We defined an indolent disease presentation as no need for CD-related surgery, hospitalization, nor initiation of steroid, immunomodulatory, or biologic therapies within the first 30 days after diagnosis, while a complicated course was defined as the opposite.
Results
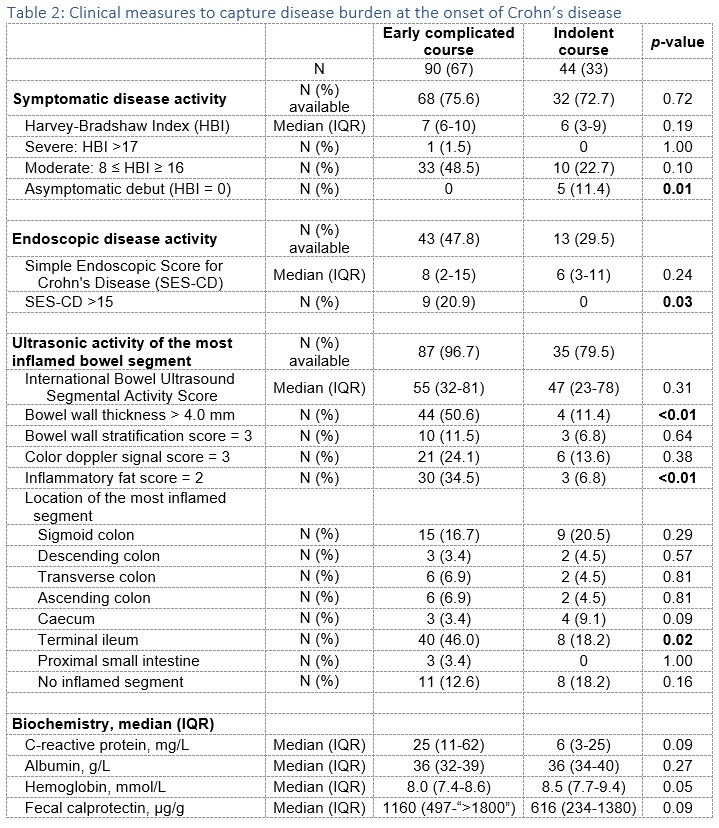
The study included 134 patients with adult-onset CD, of whom approximately one-third (44/134, 33%) had an early indolent course, with 26 patients (19%) not requiring any medication (Tables 1-2). In demographic factor adjusted analyses, a colonic phenotype (adjusted odds ratio (aOR) =4.5 (95% confidence interval (CI) 1.6-15) and a low symptom load measured with Harvey-Bradshaw Index (HBI) <5 (aOR = 3.1 (CI 1.0-10) were independently associated with an indolent course. In contrast, a C-reactive protein (CRP) level higher than 10 mg/L was the only parameter associated with a complicated onset of CD (aOR = 4.7 (CI 2.1-12)). Pearson’s correlation analyses demonstrated a significant, moderate correlation between fecal (F-) calprotectin, CRP, and endoscopic lesions, measured with Simple Endoscopic Score for CD (SES-CD) (Table 3). HBI and the International Bowel Ultrasound Segmental Activity Score (IBUS-SAS) exhibited a significant but weak correlation with CRP. In a sensitivity analysis allowing exposure to anti-inflammatory therapy for only up to seven days, the platelet count, F-calprotectin, and bowel wall thickness measured in IBUS-SAS demonstrated a significant and moderate correlation with SES-CD. The total IBUS-SAS and CRP showed a significant but weak correlation, and other measures included in the IBUS-SAS did not yield significant correlations.


Conclusion
Preliminary data from the ongoing population-based cohort indicate that one-third of patients with newly diagnosed CD have an early indolent course. This study identified colonic disease location and CRP levels to be associated with the early course, while platelet count, bowel wall thickness, and CRP were correlated with endoscopic lesions at the onset of CD.
References
1. Attauabi M et al. Immunity and the Microbiome on the Prognosis of Inflammatory Bowel Disease (IBD Prognosis Study): the protocol for a Copenhagen IBD Inception Cohort Study. BMJ Open. doi:10.1136/bmjopen-2021-055779


