P295 VALIDation of the IBD-Disk instrument for assessing disability in inflammatory bowel diseases in a population-based cohort: The VALIDate study
C. Le Berre1, A. Bourreille1, M. Flamant1, G. Bouguen2, L. Siproudhis2, M. Dewitte2, N. Dib3, E. Cesbron-Metivier3, T. Goronflot4, P.A. Gourraud4, E. Kerdreux5, A. Poinas6, C. Trang-Poisson1
1Department of Gastroenterology, CHU Hotel Dieu, Nantes Cedex 1, France, 2Department of Gastroenterology, CHU de Rennes, Rennes, France, 3Department of Gastroenterology, CHU d’Angers, Angers, France, 4Department of Biostatistics, CHU Hotel Dieu, Nantes Cedex 1, France, 5Centre d’Investigation Clinique, CHU Hotel Dieu, Nantes Cedex 1, France, 6Direction de la Recherche Clinique, CHU Hotel Dieu, Nantes Cedex 1, France
Background
Inflammatory bowel diseases (IBD) are disabling disorders. The IBD-Disability Index (IBD-DI) was developed for quantifying disability in IBD patients but is difficult to use. The IBD-Disk is a shortened and visual adaptation of the IBD-DI. It has not been validated yet. The main objectives were to validate the IBD-Disk in a large cohort of IBD patients and to assess its variability over time.
Methods
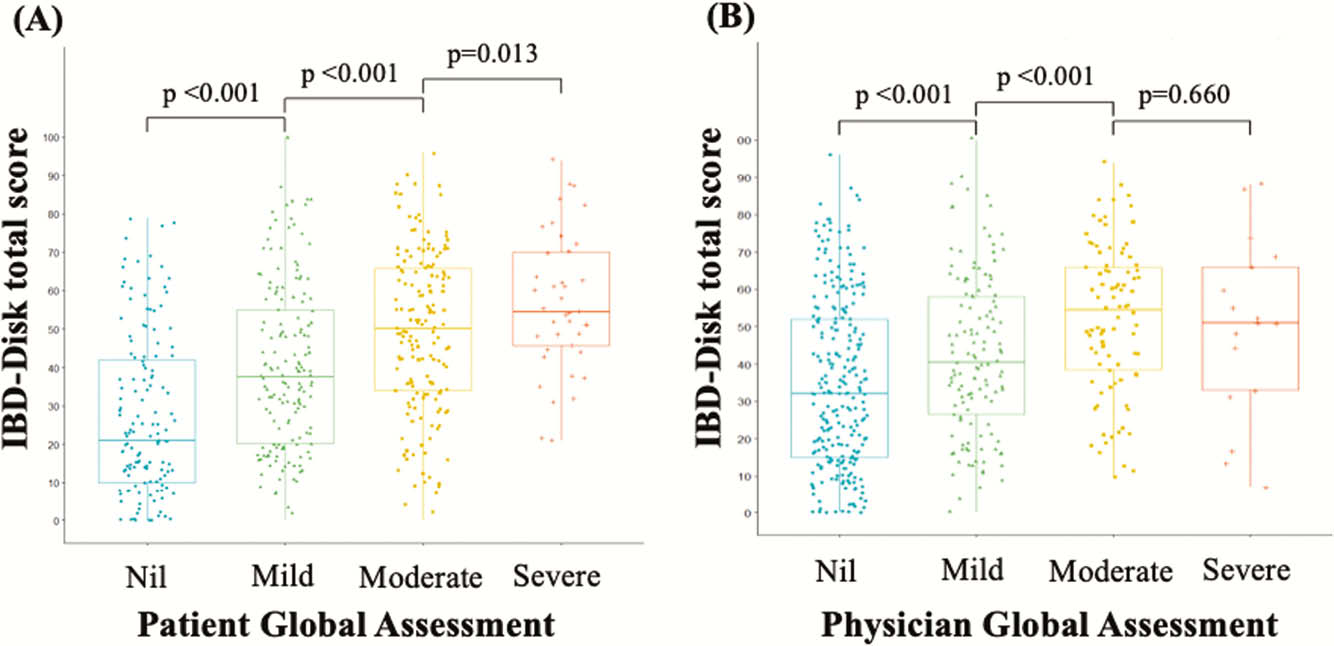
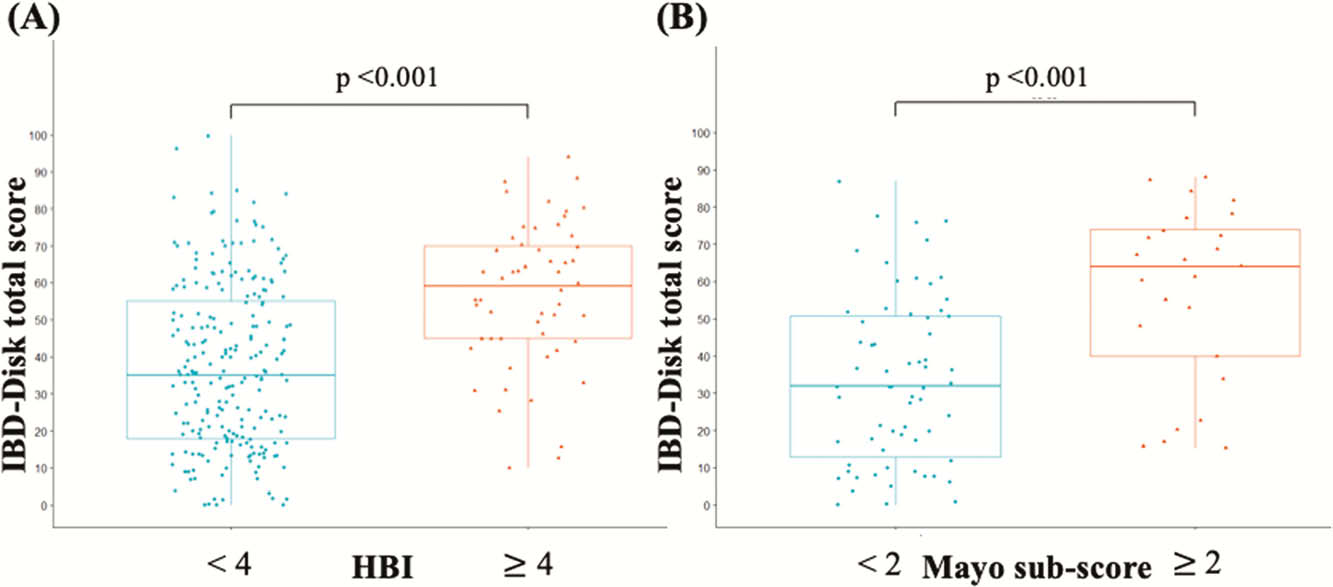
From March 2018 to July 2019, IBD patients from three university-affiliated hospitals responded twice to both IBD-Disk and IBD-DI at 3–12 months intervals (NCT03590639). Validation included concurrent validity, reproducibility, internal consistency, and evaluation of IBD-Disk correlation with IBD activity. Variability was assessed by comparing scores between baseline and follow-up visits.
Results
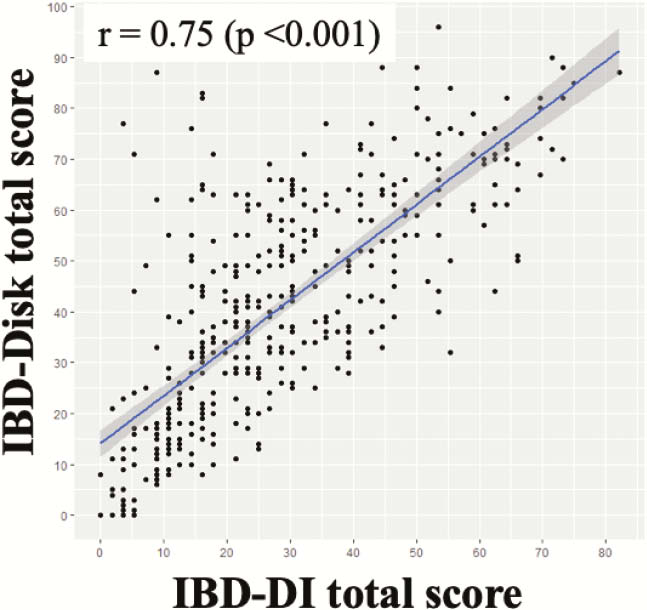
A total of 559 patients (73% Crohn’s disease, 27% ulcerative colitis) were included and 389 were followed up (Table 1). There was a good correlation between IBD-Disk and IBD-DI scores (
| Gender, | |
| Female | 313 (56) |
| Age at baseline, mean (SD) | 40.1 (14.1) |
| Age at diagnosis, mean (SD) | 28.1 (12.5) |
| Disease location (CD / UC), n (%) | |
| L1 / E1 | 114 (28) / 32 (22) |
| L2 / E2 | 103 (25) / 52 (35) |
| L3 / E3 | 187 (46) / 62 (42) |
| L4 / Pouchitis | 38 (9) / 3 (2) |
| Disease behaviour in CD, n (%) | |
| B1 | 219 (54) |
| B2 | 130 (32) |
| B3 | 58 (14) |
| Perineal location in CD, n (%) | |
| Never | 295 (72) |
| Past | 84 (21) |
| Active | 28 (7) |
| Extra-intestinal manifestation, n (%) | 123 (22) |
| Intestinal resection, n (%) | 172 (31) |
| Stoma, n (%) | 25 (4) |
| Perianal surgery, n (%) | 85 (15) |
| Seton, n (%) | 7 (1) |
Conclusion
This is the first study to validate the IBD-Disk in a large cohort of IBD patients, demonstrating that it is a valid and reliable tool for quantifying disability in clinical practice. Further studies are warranted to assess its correlation with endoscopic activity, to explore its responsiveness to change, and to evaluate the factors associated with disability.


