P310 Is ileoanal pouch excision a destination therapy for Inflammatory Bowel Disease? Data from a quaternary pouch referral center
Choi, S.(1);Lightner, A.(1);Lipman, J.(1);Hull, T.(1);Steele, S.(1);Holubar, S.(1);Rieder, F.(2);
(1)Cleveland Clinic Foundation, Colorectal Surgery, Cleveland, United States;(2)Cleveland Clinic Foundation, Gastroenterology, Cleveland, United States
Background
Although ileal pouch-anal anastomosis (IPAA) is the surgical procedure of choice of many patients with ulcerative colitis and other conditions, some patients may require pouch excision (PEx). We aimed to describe our experience with pouch excisions and associated outcomes with an emphasis on late medical, endoscopic, and surgical interventions for inflammatory bowel disease (IBD).
Methods
We performed a retrospective review of a prospective colorectal surgery database. All pouch excisions performed at our quaternary pouch center from 2006 – 2019 were included; pelvic exenteration, PEx with neo-IPAA or Kock-pouch were excluded. Early complications occurred <30 days, late complications >30 days. Medications taken prior to PEx were included if taken within 12 weeks of pouch excision. Data are reported in frequency (proportion) or median (interquartile range).
Results
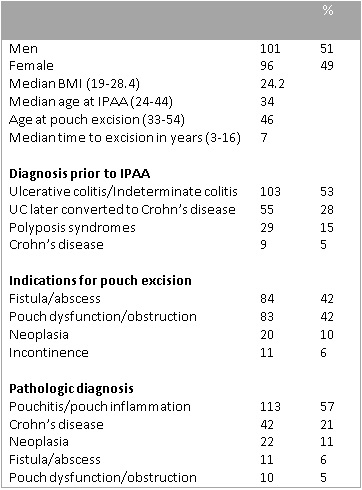
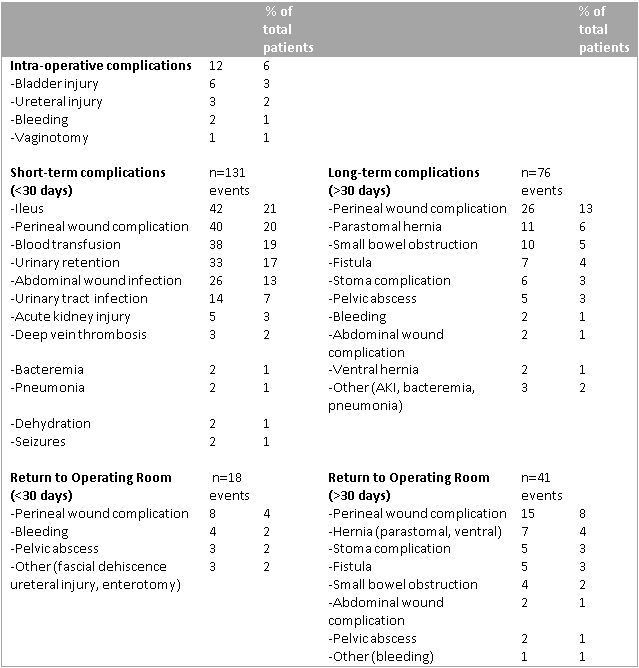
A total of 197 cases met inclusion criteria, and were performed by 23 surgeons, median 6 excision (IQR 2 - 14) cases over a 14-year period: of these, 105 had their index pouch created at our quaternary pouch referral center (overall PE rate 2.7%). Indications for PEx are shown in Table 1. Median time to PEx was 7 years and 94 (48%) patients had re-diversion prior to PEx. Medications prior to PEx: 34 (17%) steroids, 27 (14%) biologics, and 22 (11%) immune-modulators. The median duration of surgery was 4 hours (3.2-5). The median estimated blood loss was 263 ml (150-500) with 24 patients (12%) requiring at least one unit of packed red blood cells intra-operatively. Most pouch excisions were done through laparotomy; 2 cases (1%) were started robotically and 11 cases (10%) laparoscopically with a 26% conversion rate. Intersphincteric dissection was used in 172 cases (87%) while 26 cases (13%) required abdomino-perineal resection, of which 58% had a neoplastic indication. Intra-operative, early and late complications are shown in Table 2; 40 patients (20%) had perineal wound complications in less than 30 days, while 26 patients (13%) had long-term perineal wound complications, of which 15 patients required return to the operating room. After PEx, 23 patients out of 167 patients (14%) required continuation of IBD medications, 6 patients (3.6%) required surgery, and 4 patients (2.4%) required endoscopic intervention for their IBD.
Conclusion
In this large series of ileoanal pouch excisions, we found that perineal wound complications are common, but infrequently require operative intervention. For most IBD patients in this series, pouch excision did appear to be a destination therapy for IBD with a small minority requiring ongoing medical therapy for IBD.