P314 Microscopic appendicitis in ulcerative colitis: Feasibility of ultrasonographic diagnosis
Reijntjes, M.(1)*;Pruijt, M.(2);Visser, E.(1);de Voogd, F.(2);d'Haens, G.R.(2);Mookhoek, A.(3);Gecse, K.B.(2);Buskens, C.J.(1);Bemelman, W.A.(1);
(1)Amsterdam University Medical Centers, Surgery, Amsterdam, The Netherlands;(2)Amsterdam University Medical centers, Gastroenterology, Amsterdam, The Netherlands;(3)Institute of Pathology- University of Bern, Pathology, Bern, Switzerland;
Background
Increasing evidence suggests appendectomy as potential alternative treatment in patients with ulcerative colitis (UC), especially in those with histological appendiceal inflammation (AI). Intestinal ultrasound (IUS) is a non-invasive diagnostic modality that detects differences in the appendix between UC patients and healthy controls1. This study aimed to correlate appendiceal IUS and endoscopic findings to histopathological inflammation in resection specimens of UC patients undergoing appendectomy.
Methods
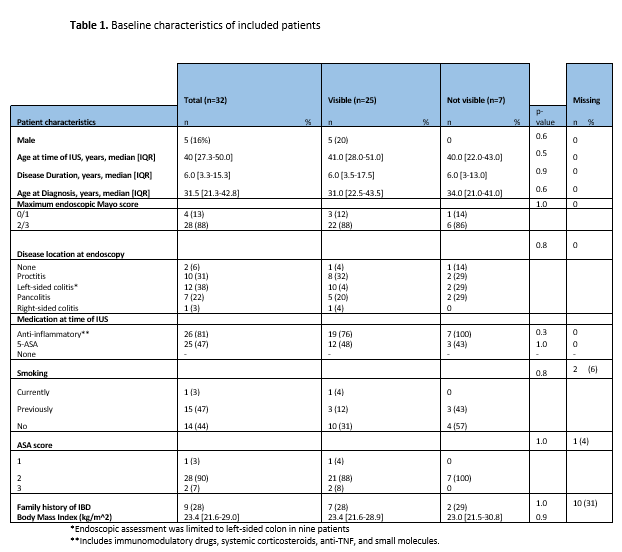
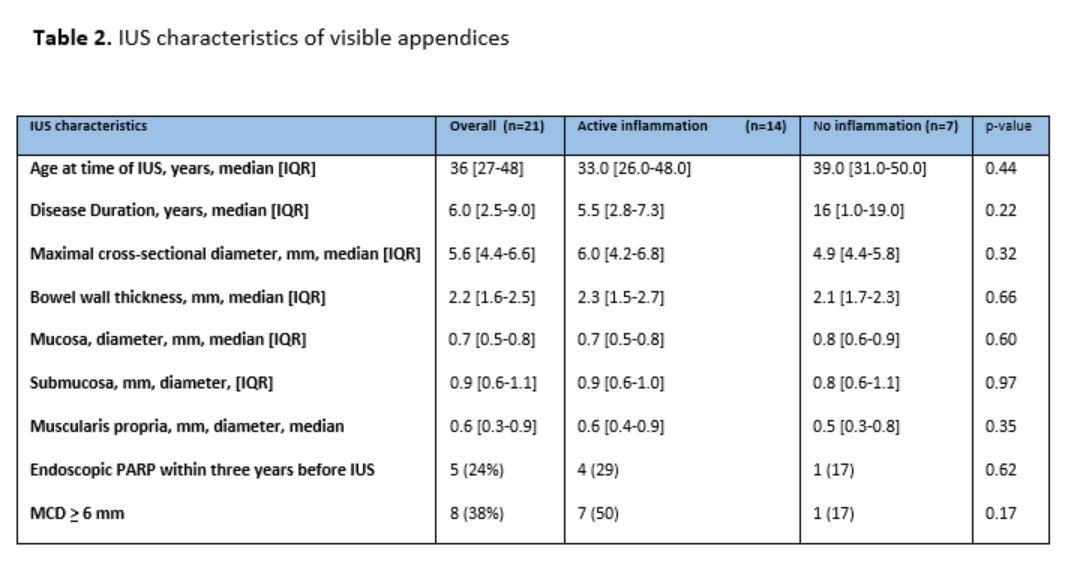
In this prospective cohort study, appendiceal IUS was performed in UC patients undergoing endoscopy and subsequent appendectomy between 2020 and 2022 in a trial for UC (NCT03912714). Primary outcome was the correlation between an increased maximal cross-sectional diameter (MCD, ≥ 6 mm) and AI in patients with a visible appendix on IUS. Presence of AI was assessed in pathology reports. Patients with fibrosis (F) were excluded from IUS analyses. Secondary outcomes included bowel wall thickness (BWT) on IUS and presence of endoscopic peri-appendiceal red patch (PARP) before appendectomy.
Results
In total, 32 UC patients who underwent laparoscopic appendectomy in study setting were included (84% female, median age 40 [IQR 27-50] years). The majority of patients demonstrated left sided disease (38%) and a mayo score ≥ 2 (88%) on baseline endoscopy. A median window between ultrasound and appendectomy of 1.2 (0.1-2.1) months was found. A total of eighteen (56%) patients were demonstrated to have AI in the resection specimen, and five (16%) patients demonstrated F. The appendix was visualised on IUS in 25 (78%) UC patients, with no difference in patients with AI (AI: 78%, no AI: 78%, p= 1.0). The overall median MCD and BWT were 5.6 [IQR 4.4-6.6] and 2.2 [1.6-2.5] mm, respectively. Patients with AI demonstrated a numerically higher median MCD (AI: [6.0 [4.2-6.8], no AI: 4.9 [4.4-5.8] mm, p= 0.3). Patients with an increased MCD were more likely to demonstrate pathologic AI, although not significant (OR: 6.0, CI 95%: 0.6-63.7, p=0.1). A minority of patients with AI demonstrated to have an endoscopic PARP: 5/18 (28%). The median MCD of patients with PARP was numerically higher (PARP: 6.0 [IQR 4.4-7.8] vs no PARP: 5.5 [4.0-6.6], p=0.5).
Conclusion
IUS is a feasible modality for assessment of the appendix. Although significance was not reached, patients with an increased MCD were more likely to demonstrate AI.
1Reijntjes MA, de Voogd FAE, et al. Intestinal ultrasound detects an increased diameter and submucosal layer thickness in the appendix of patients with ulcerative colitis compared to healthy controls - a prospective cohort study. Aliment Pharmacol Ther. 2022 Nov 1.