P344 Diverting ileostomy in Inflammatory Bowel Disease's surgery: the real clinical cost analysis
Ascari, F.(1)*;Barugola, G.(2);Ruffo, G.(2);
(1)Ospedale di Carpi AUSL Modena, Chirurgia Generale, Carpi Modena, Italy;(2)IRCCS Sacro Cuore Don Calabria, Chirurgia Generale, Negrar di Valpolicella Verona, Italy;
Background
A loop ileostomy does not prevent an anastomotic leak and it is not risk-free, but it can decrease the clinical impact of dehiscence. Inflammatory bowel disease condition is more complex than other benign situations candidated to colorectal surgery. The aim of our study was to assess the risk of complications related to the stoma presence and to identificate variables related with complications in a series of IBD’s patients undergoing various colorectal surgeries along with primary diverting stoma.
Methods
We conducted a retrospective study of patients who underwent sphincter-preserving elective surgery for IBD between January 2014 to December 2020 at IRCCS Sacro Cuore Don Calabria Hospital. Data were collected regarding baseline demographics, operative techniques and complications. Ileostomy-related complications were separated into three categories: complications related to stoma creation at the time of index surgery within 30 days; complications of having an ileostomy; complications of ileostomy closure.
Results
Fifty-six diverting loop ileostomies were performed and included in our study (table 1). Seventeen patients (30%) at index procedures had the following complications: 5 had anastomotic leak or pelvic abscess (8.9%), 3 had bowel obstruction (5.4%) and 7 (12.5%) bleeding requiring transfusion. Two patients had complications related to ileostomy creation: 1 had prolapse (1.8%) and 1 rotation with obstruction (1.8%). Seven patients (12.5%) required reoperation. Seven patients (12.5%) were readmitted within 30 days after index surgery for dehydratation. Twenty-four patients (42.1%) suffered during the same time from ileostomy management’s problems. Eighteen patients (32.1%) at stoma closure had the following complications: 6 had anastomotic leak or pelvic abscess (10.7%), 7 had SSI (12.5%), 5 had bowel obstruction (8.9%) and 2 bleeding requiring transfusions (3.6%). Nine patients (16%) required reoperation. At univariate analysis complications of ileostomy status are more frequent in male (p=0.01) and in patients who had ileostomy creation complications (p=0.04). Ileostomy closure complications are more common in male patients (p=0.005). Complications at the time of ileostomy creation were found at multivariate analysis statistically related to complications during ileostomy maintenance.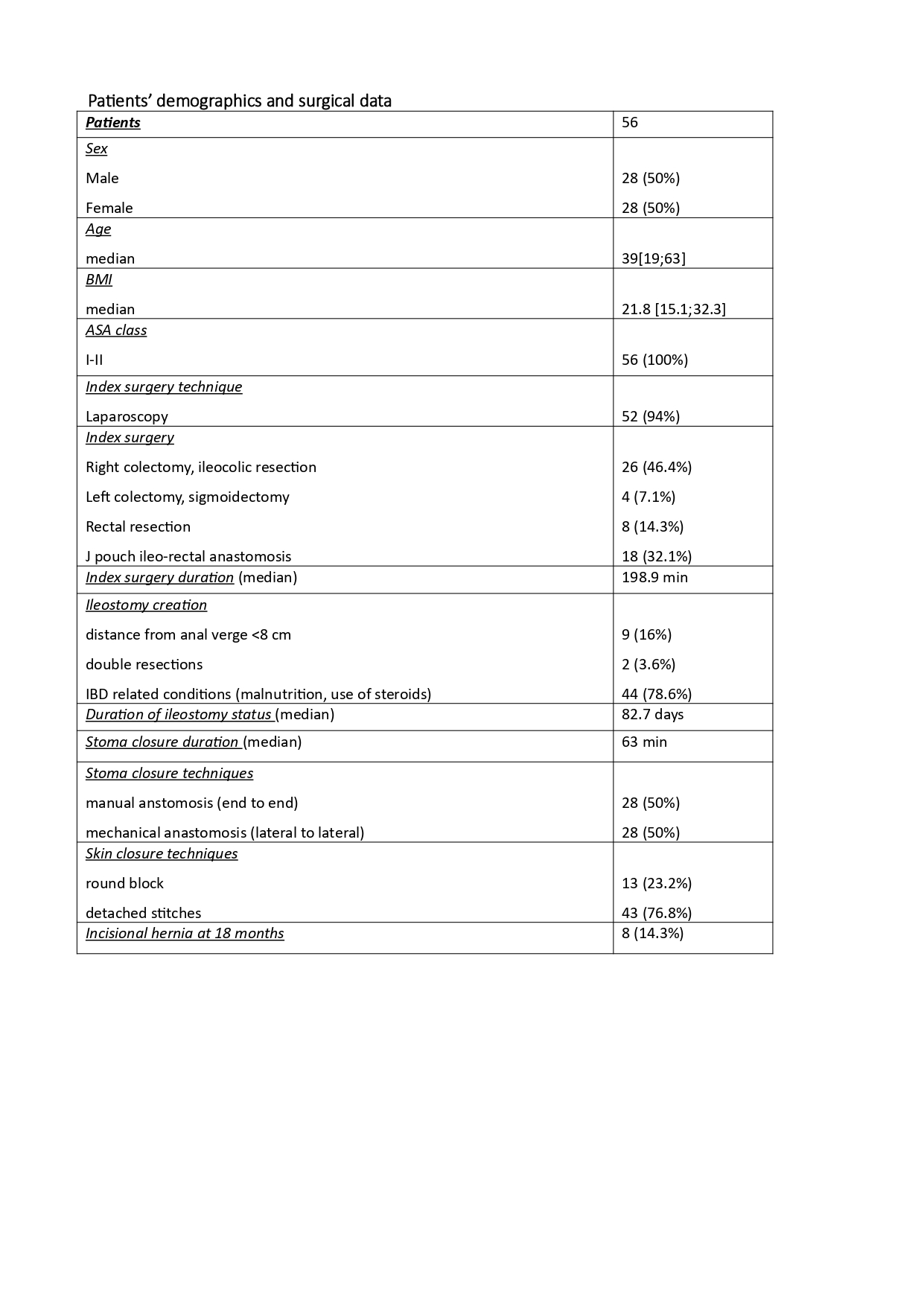
Conclusion
Ileostomy alone cannot mitigate the overall high rate of complications expected in IBD’s patients, also in consideration of potential problems stoma it-self related. Even if our study is retrospective and presents a small court, when resection is necessary despite patient's conditions we propose to resect without anastomosis at the time of index procedure and restore the bowel continuity only after patient's status optimization.


