P358 Predictors of response to faecal microbiota transplantation in patients with active ulcerative colitis
A. Singh1, A. Sood1, V. Midha2, R. Mahajan1, N. Bansal3, K. Kaur4, D. Singh3
1Department of Gastroenterology, Dayanand Medical College and Hospital - Ludhiana, Ludhiana, India, 2Department of Medicine, Dayanand Medical College and Hospital - Ludhiana, Ludhiana, India, 3Research and Development Centre, Dayanand Medical College and Hospital - Ludhiana, Ludhiana, India, 4Department of Pharmacology, Dayanand Medical College and Hospital - Ludhiana, Ludhiana, India
Background
Faecal microbiota transplantation (FMT) has been shown to be effective for induction of remission in nearly 50% patients with active UC. At present, factors impacting the response to FMT in UC remain unclear.
Methods
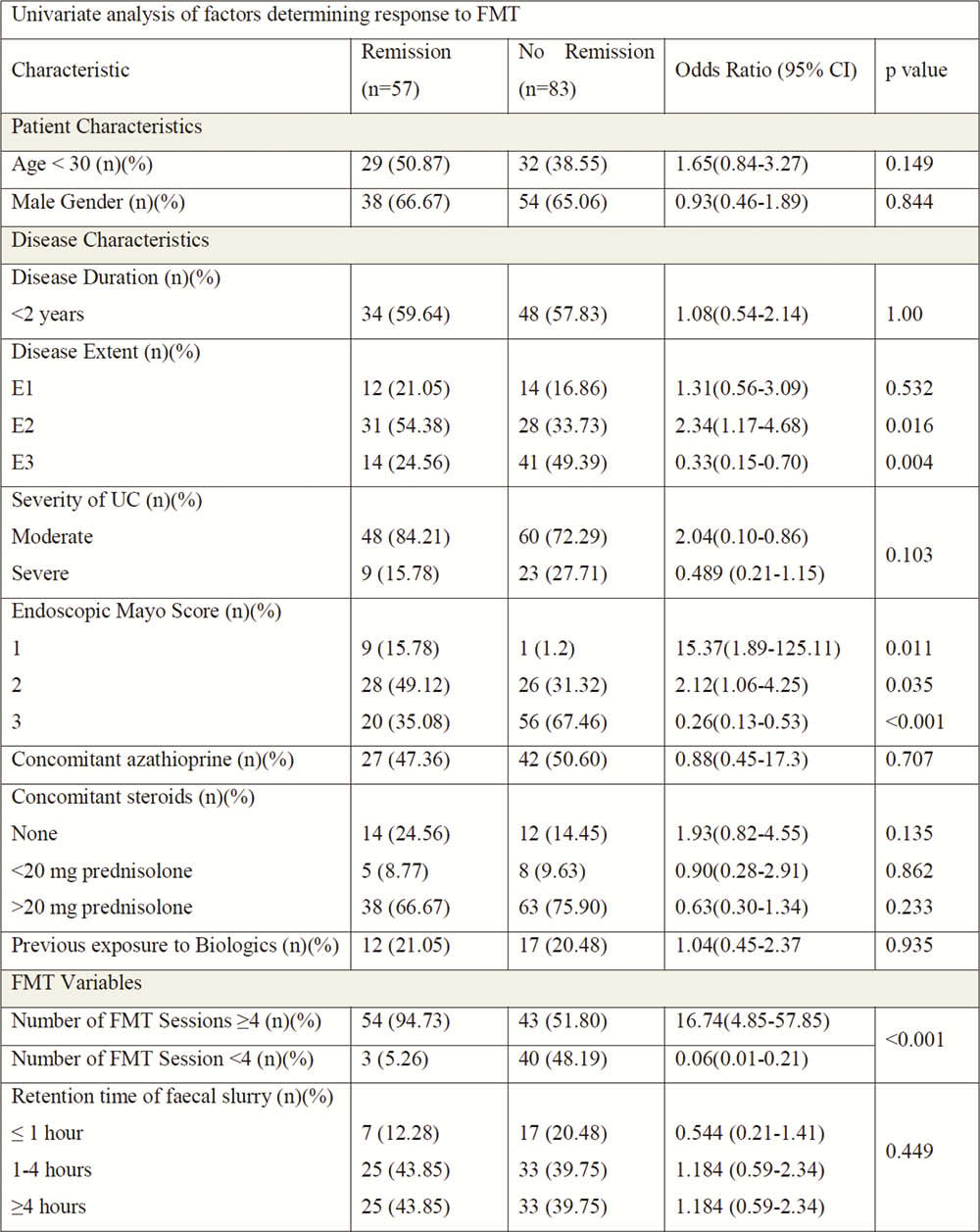
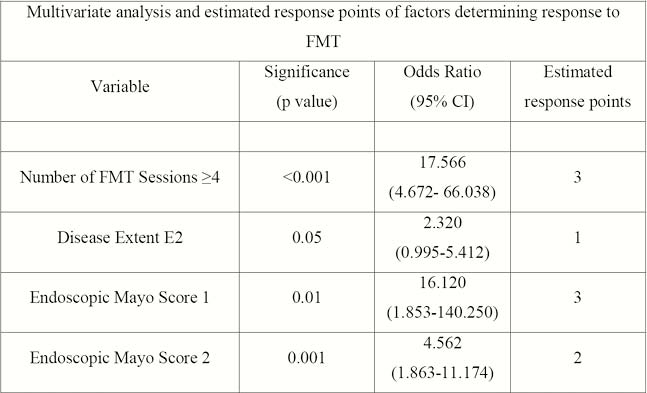
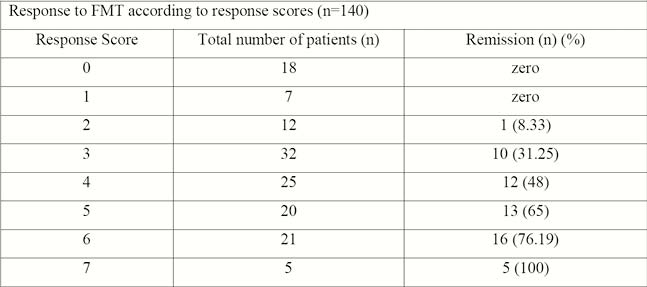
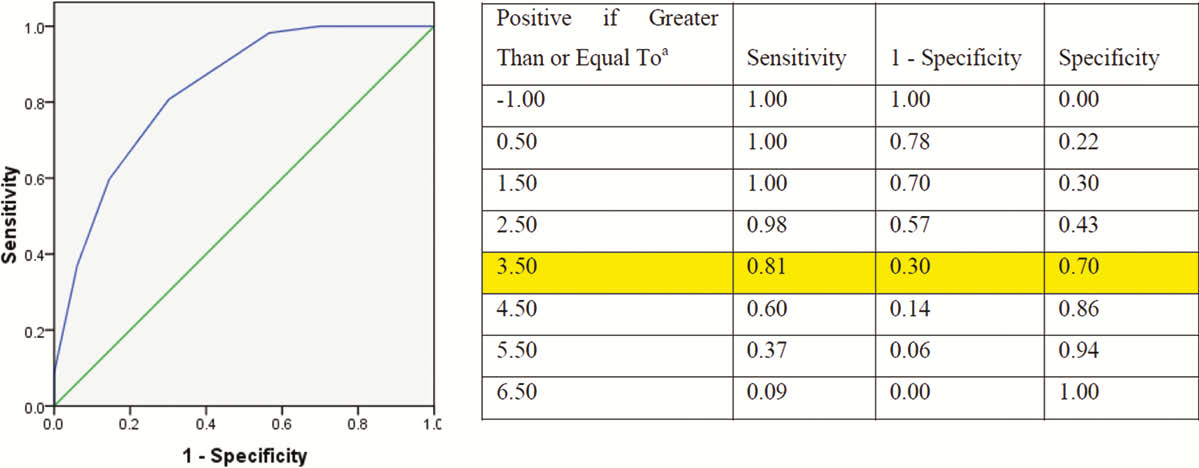
Patients with active UC treated with FMT via colonoscopy at weeks 0, 2, 6, 10, 14, 18, and 22 between September 2015 and March 2019 were analysed. Response to FMT was defined as achievement of clinical remission (Mayo score ≤2, with each sub-score ≤ 1 and endoscopic subscore of 0) at week 22. Patient and disease characteristics and FMT-related factors, considered to affect response to FMT were evaluated in a multivariable logistic regression analysis to determine the predictors of response to FMT. A statistical model was subsequently developed for predicting the success of FMT.
Results
Out of 140 patients with active UC and treated with FMT [mean age 34.29 ± 11.51 years, 65.71% males (
| Mean age (years) (mean ± SD) | 34.29 ± 11.51 |
| Males ( | 92 (65.71) |
| Disease duration (years) (mean ± SD) | 4.71 ± 4.57 |
| Disease extent ( | |
| E1 | 26 (18.57) |
| E2 | 59 (42.14) |
| E3 | 55 (39.28) |
| Disease Severity ( | 108 (77.14)32 (22.86) |
| Mayo score (mean ± SD) | 7.8 ± 2.26 |
| Endoscopic Mayo score (mean ± SD) | 2.47 ± 0.62 |
| Number of FMT sessions (n) (mean ± SD) | 5.37 ± 2.68 |
| Faecal slurry retention time (h) (mean ± SD) | 3.11 ± 1.63 |
| Concomitant medications ( | |
| 5-ASA | 140 (100) |
| Azathioprine | 69 (49.28) |
| Corticosteroids | 114 (81.42) |
| Biologics | Nil |
| Previous exposure to biologics (n) (%) | 29 (20.71) |
Conclusion
Disease Extent E2, endoscopic mayo score 1 or 2, and number of FMT sessions ≥4 predict response to FMT in active UC. The prediction model has good discriminative power at identifying individuals likely to respond to FMT.


