P361 The effect of immunomodulators and other factors on the persistence of biological agents for Crohn’s disease and ulcerative colitis: data from the Australian population-based registry
Y. Ko1,2, S. Paramsothy1,2, R. Leong1,2
1Gastroenterology and Liver Services, Concord Repatriation General Hospital, Sydney, Australia, 2Concord Clinical School, University of Sydney, Sydney, Australia
Background
Treatment persistence (duration of medication use) provides real-world evidence on therapeutic effectiveness, tolerability and prescriber and patient preferences. Biological agent persistence in Crohn’s disease (CD) and ulcerative colitis (UC) was compared from a national population-based registry with no hierarchical prescribing order. We hypothesised immunotherapy co-therapy would increase persistence for anti-TNF agents, but not for non-anti-TNF agents due to reduced immunogenicity.
Methods
A randomly selected ten per cent subgroup of the prospectively collected population-based registry from the Australian Pharmaceutical Benefits Scheme between June 2005 and June 2019 was analysed. Treatment persistence of adalimumab (ADA), infliximab (IFX), vedolizumab (VDZ) and ustekinumab (UST) was compared. Factors affecting discontinuation were evaluated using multivariate proportional hazard regression.
Results
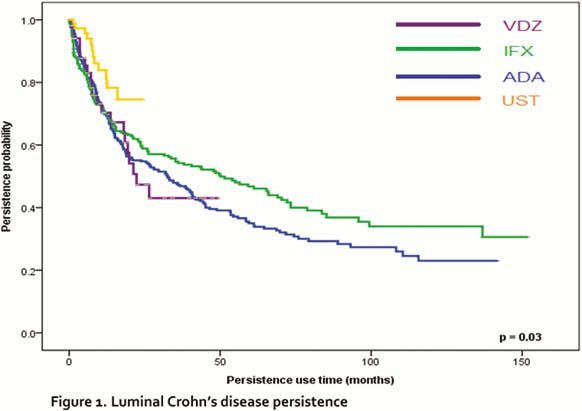
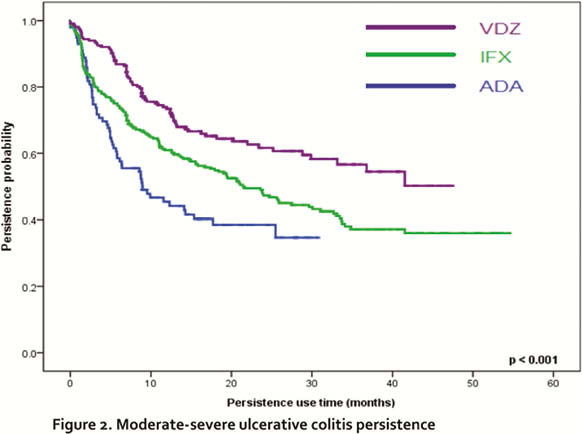
886 patients consisting of 1294 lines of therapy (992 CD, 302 UC, 2778 person-years of follow-up) were included. In CD, UST had the highest overall persistence rate (median persistence rate was > 74.6% where 24.6 months is the maximum follow-up time recorded), followed by VDZ, IFX and ADA (
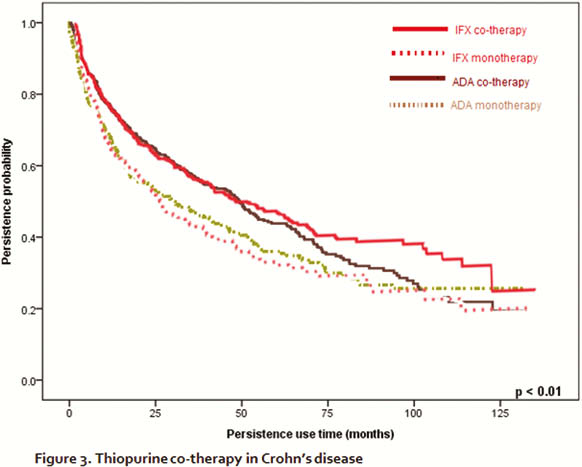
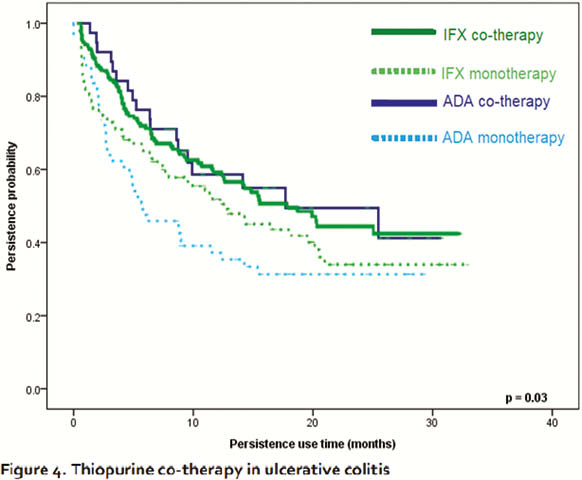
Persistence of biological agents correlated with immunomodulator co-therapy in CD (
On multivariate analysis, higher persistence was seen in males (HR: 0.75 95% CI: 0.59–0.94) and with immunomodulator co-therapy (HR 0.77 95% CI: 0.61–0.97,
Conclusion
This real-world data reflecting treatment effectiveness, tolerability and patient and prescriber preferences supports the use of UST and VDZ over anti-TNF agents in CD and UC, respectively, to achieve high treatment persistence which is independent of immunomodulator co-therapy, possibly secondary to differing immunogenicity rates. It also highlights the substantial increase in anti-TNF therapy persistence with thiopurine co-therapy, but not with methotrexate.


