P394 A prospective analysis of body composition in patients with Inflammatory Bowel Disease and changes during biologic therapy
Nguyen, A.(1);Burns, M.(2);Herath, M.(3);Holt, D.(2);Gibson, P.R.(4);Milat, F.(3);Ebeling, P.(5);Moore, G.(6);
(1)Monash University- Monash Health and Alfred Health, Gastroenterology, Melbourne, Australia;(2)Monash Health, Gastroenterology, Melbourne, Australia;(3)Monash University- Monash Health and Hudson Institute of Medical Research, Endocrinology, Melbourne, Australia;(4)Monash University and Alfred Health, Gastroenterology, Melbourne, Australia;(5)Monash University and Monash Health, Endocrinology, Melbourne, Australia;(6)Monash University and Monash Health, Gastroenterology, Melbourne, Australia;
Background
Low muscle mass is common in Inflammatory Bowel Disease (IBD) and is associated with poor quality of life and increased need for surgery. Our aim was to compare body composition in patients with IBD to controls, active and inactive IBD, and before and after biologic induction therapy.
Methods
Body composition was prospectively analysed in patients with IBD and gender-matched controls. Active disease was defined as a faecal calprotectin (FCP) ≥150 µg/g. In patients with active IBD commencing biologic therapy, body composition was measured at baseline and after induction, at ≥14 weeks. Patients were considered responders if the FCP reduced by ≥50%. All participants underwent whole-body dual-energy X-ray absorptiometry (DXA) (GE Lunar Prodigy), hand-grip strength, an International Physical Activity Questionnaire, Australian Eating Survey and a Subjective Global Assessment for malnutrition. Low skeletal muscle index (SMI) was defined as men ≤7.26 kg/m2 and women ≤5.45 kg/m2. Protein intake <15% of total daily macronutrient intake was considered low.
Results
Patients with IBD (54% Crohn’s disease, 56% male) had a median age of 29 years (IQR 23-40) and 5-year duration of disease (IQR 1-11). Body composition was similar between 48 patients with IBD and 30 controls, including body mass index (25 vs 23 kg/m2), fat mass (24.5 vs 18.7 kg), estimated visceral adipose tissue (437 vs 318 g), total lean body mass (46.6 vs 47.9 kg) and appendicular skeletal mass (21.3 vs 23.2 kg). 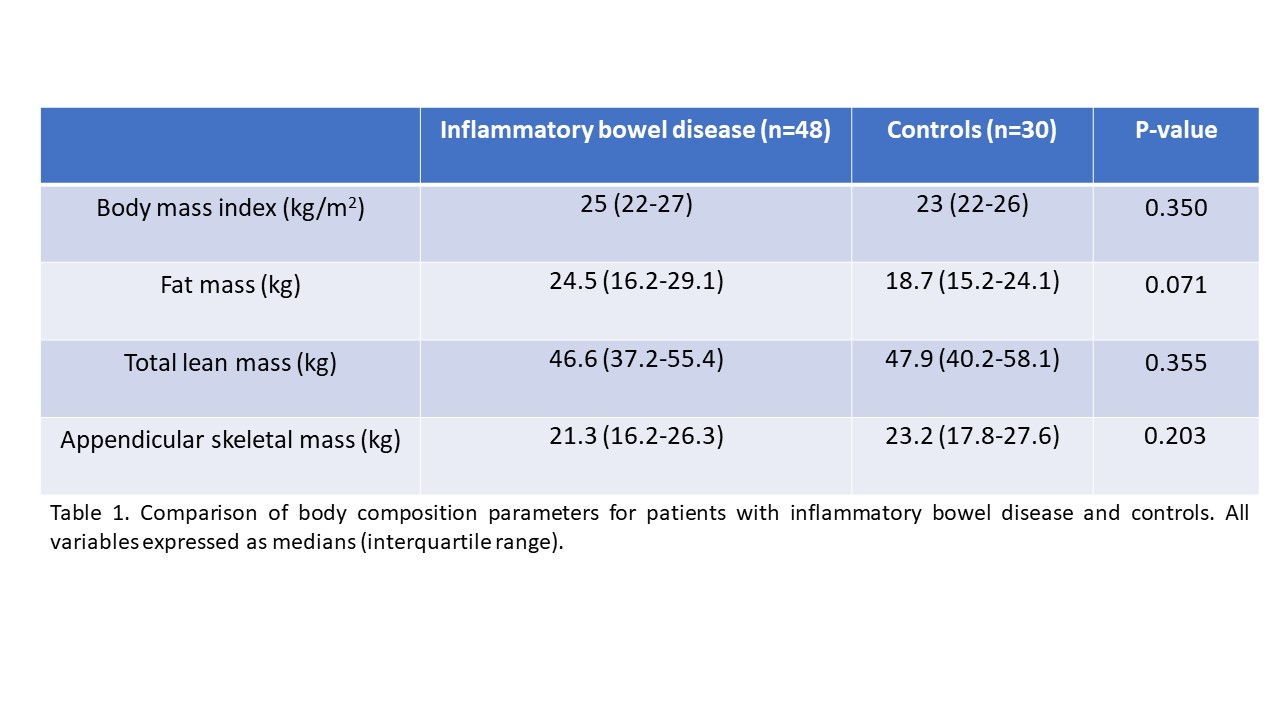
These markers were also similar when comparing active (n=28) to inactive (n=16) patients with IBD, stratified by gender. Low SMI was more common in the IBD cohort compared to controls (19% vs. 3%, p=0.048). Only one patient with low SMI had low hand-grip strength to meet the criteria for sarcopenia in the IBD cohort. More patients with IBD had low protein intake (13% vs 0%, p=0.027) and were mild to moderately undernourished (25% vs 0%, p=0.003) compared to controls. No difference was found with physical activity and hand-grip strength. In the IBD cohort, patients with low SMI were more likely to be undernourished (56% vs 18%, p=0.019) but had similar protein intake compared to those with normal SMI. In 7 of 14 patients who responded to biologic therapy, SMI (7.9 to 9 kg/m2, p=0.028) and total lean body mass (50.6 to 54.3 kg, p=0.043) increased, while total fat mass or body mass index did not change. Low SMI was found in 3 responders at baseline and increased after induction. There was no change in any body composition parameters in non-responders (n=7).
Conclusion
Body composition was similar between patients with IBD and controls, however low SMI was more common in IBD. Increasing muscle mass can be detected at ≥14 weeks after active disease is treated.


