P401 Concomitant azathioprine treatment effects vedolizumab treatment persistence in Crohn's Disease but not in Ulcerative Colitis
Toruner, M.(1)*;Guvenir, T.(1);Er, R.E.(1);Soykan, I.(1);
(1)Ankara University School of Medicine, Department of Gastroenterology, Ankara, Turkey;
Background
Vedolizumab is a monoclonal antibody against integrin α4β7 that is being used for the treatment of moderate to severe Ulcerative Colitis (UC) and Crohn’s Disease (CD). Recent studies have shown conflicting results for the effect of concomitant azathioprine use with vedolizumab monotherapy. In this single center cohort study, we investigated the effect of concomitant azathioprine treatment on vedolizumab drug persistence in UC and CD treatment.
Methods
We performed a retrospective review of all adult (≥18 years) UC and CD patients started on VDZ at our infusion center. Data collection included baseline demographics, concomitant azathioprine therapy, VDZ therapy and disease activity scores using the partial Mayo score and Harvey Bradshaw Score. Data were obtained from the digital medical record. The primary outcome measure was VDZ persistence, represented in Kaplan-Meier analysis. This analysis assessed persistence on every 8 week dose regimen.
Results
This single center cohort included 142 VDZ treated UC (n=64) and CD (n=78) patients. All patients had a history of at least one anti-TNF treatment: Mean age 38.9±12.5 years and male gender 84 (59.2%). Median disease duration was 6±1.6 years. 6 Patients were excluded from the analysis since VDZ therapy has been stopped due to side effects. Mean duration of VDZ treatment in Crohn's disease was 96.5±69.2 weeks and in UC was 72.1±60.5 weeks. Concomitant azathioprine therapy in CD increased VDZ persistence rate. However, in UC concomitant azathioprine therapy did not effect VDZ persistence rate.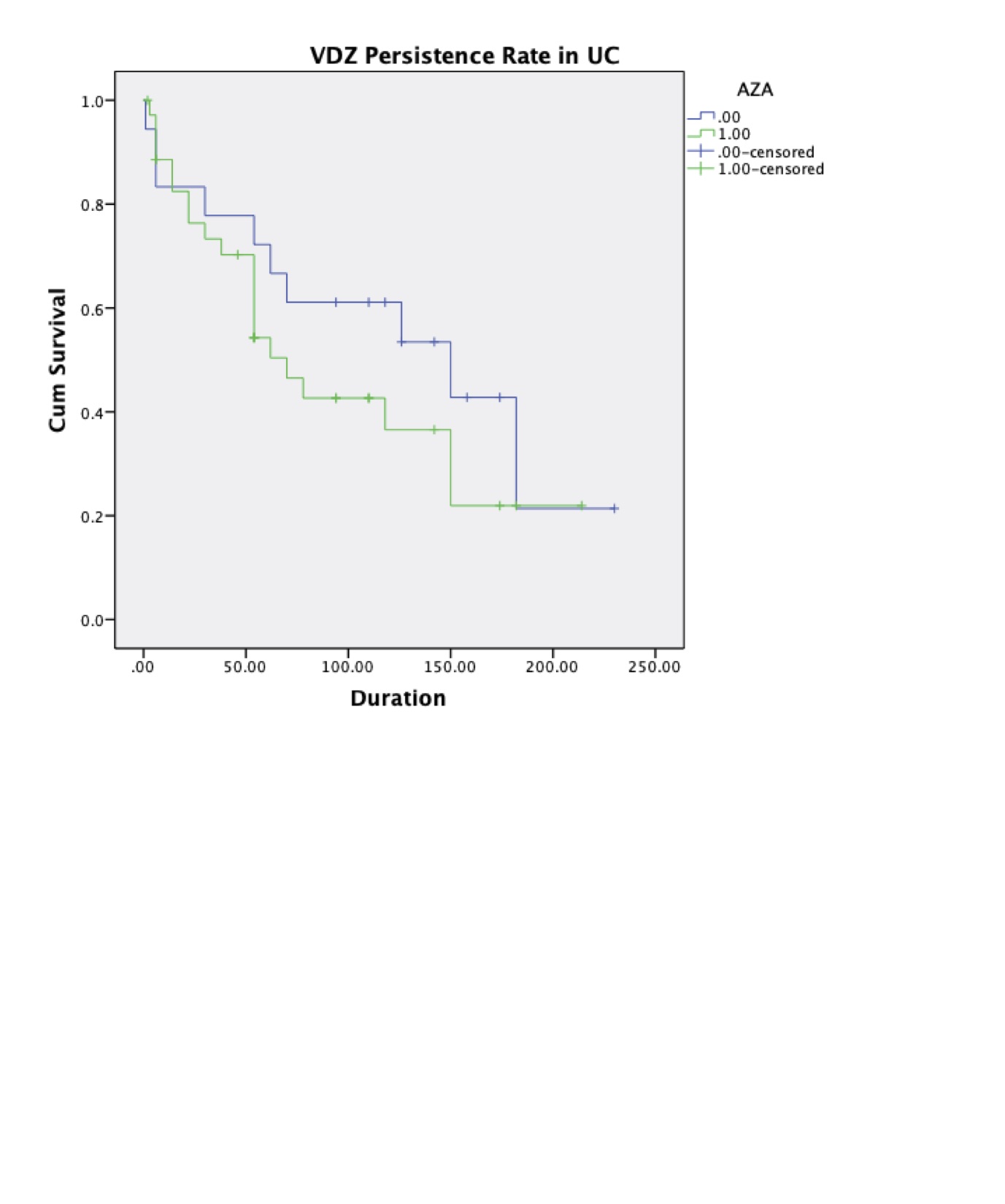

Conclusion
The real-world data collected in this study demonstrate that concomitant azathioprine treatment increase the VDZ persistence rate in Crohn's disease. However, concomitant azathioprine treatment does not effect the VDZ persistence rate in UC patients.


