P408 Faecal infliximab and disease activity in Acute Severe Ulcerative Colitis
Shields, S.(1);Dunlop, A.(2);Gerasimidis, K.(3);Nichols, B.(3);Galloway, P.(2);Macdonald, J.(1);Hansen, R.(4);Seenan, J.P.(1);
(1)Queen Elizabeth University Hospital, Gastroenterology, Glasgow, United Kingdom;(2)Queen Elizabeth University Hospital, Biochemistry, Glasgow, United Kingdom;(3)University of Glasgow, School of Medicine- Dentistry & Nursing, Glasgow, United Kingdom;(4)Royal Hospital for Children, Gastroenterology, Glasgow, United Kingdom;
Background
Infliximab (IFX) is increasingly used in the management of moderate to severe ulcerative colitis (UC) and as a ‘rescue’ treatment for acute severe UC (ASUC) but primary non response (PNR) and colectomy rates remain significant. Reasons for IFX treatment failure in ASUC are multifactorial but immunogenicity and faecal loss of drug are thought to be important factors. Emerging evidence suggests accelerated ‘rescue’ IFX dosing may be more effective. The aim of this work was to establish if a relationship exists between faecal IFX levels, disease activity, and clinical outcomes early in IFX treatment.
Methods
Patients with UC were prospectively recruited following initiation of IFX and designated as ASUC or non-ASUC based on Truelove and Witt’s criteria. Stool and serum were collected on days 0, 7, 14, 28 and 42 after initiation of IFX. Additional samples on days 1-5 after IFX were obtained from inpatients. Albumin and CRP results were extracted from electronic patient records. Faecal calprotectin (FC) was measured using ELISA (CALPROLAB). Faecal IFX within the first 2 weeks of treatment was analysed using a Promonitor-IFX-1DV ELISA assay, performed on the Triturus ELISA instrument. R studio was used to calculate areas under the curves of the time series. Spearman's rank correlation test was used for correlation analysis.
Results
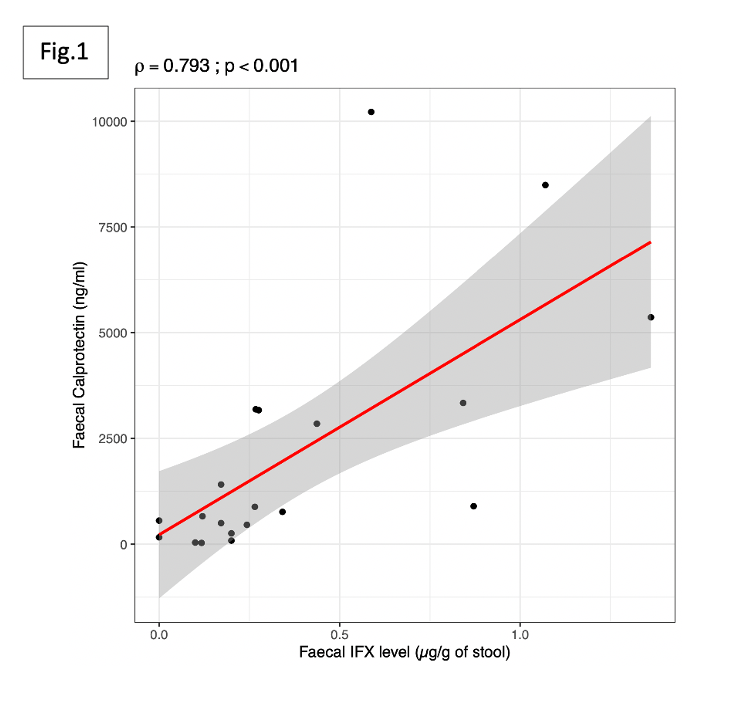
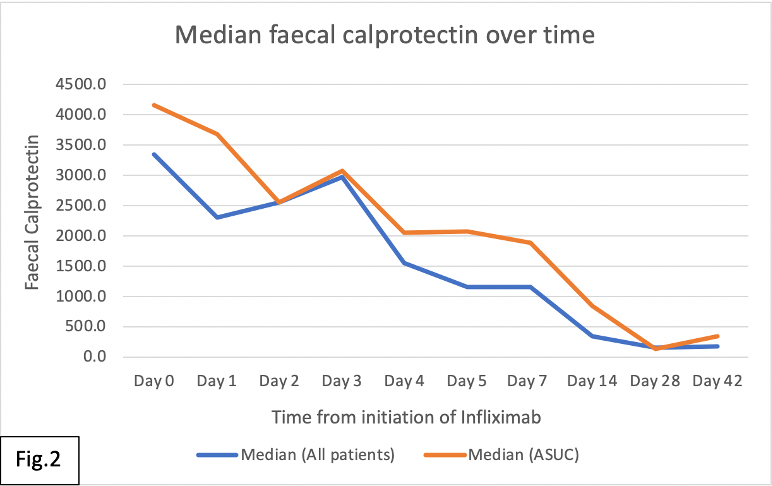
20 patients were recruited, 12 with ASUC. Faecal IFX correlated strongly with FC (ρ=0.793;p<0.001) (Fig. 1), and moderately with CRP (ρ=0.51;p=0.02), and serum albumin (ρ=-0.51;p=0.02). The correlation was strongest between faecal IFX and FC within in the first week (ρ=0.93;p<0.001), and less strong for crp (ρ=0.481;p=0.037) and albumin (ρ=-0.474;p=0.04). Higher faecal IFX was associated with increased colectomy and PNR rates but this did not reach statistical significance (p=0.098). A rapid decline in median FC was seen after initiation of IFX with a rebound rise in FC observed at day 3 of IFX treatment (Fig. 2).
Conclusion
In this small cohort, faecal loss of IFX was associated with increased markers of systemic and luminal inflammation. Its role as a biomarker for disease severity, treatment response and clinical outcomes warrants further investigation. The rapid fall but early rebound rise in FC may support the need for earlier accelerated dosing in ASUC. However, larger studies are needed to establish the optimal early IFX regime to improve clinical outcomes.
References
Papamichael et al. Aliment Pharmacol Ther 2018;47:478–484.
Hindryckx et al. Aliment Pharmacol Ther. 2017 March;45(5): 617–630
Brandse et al. Gastroenterology. 2015 Aug;149(2):350-5


