P417 Do ACE inhibitors and angiotensin II receptor blockers improve disease outcomes in inflammatory bowel disease?
K. FAIRBRASS1, D. Hoshen1, A.C. Ford1,2, D. Gracie1
1Leeds Gastroenterology Institute, Leeds Teaching Hospitals NHS Trust, Leeds, UK, 2Leeds Institute of Medical Research at St. James’s, University of Leeds, Leeds, UK
Background
The renin-angiotensin system (RAS) has an established role in the pathogenesis of fibrosis and inflammation in renal and cardiovascular disease. High concentrations of angiotensin-converting enzyme (ACE) and renin are found in the small and large bowel. This is elevated further within inflamed colonic tissue of inflammatory bowel disease (IBD) patients, compared with controls. (1) ACE inhibitor (ACEi) or angiotensin II receptor blocker (ARB) therapy may inhibit the effects of RAS in IBD. We aimed to examine the relationship between ACEi/ARB use and longitudinal disease activity outcomes in patients with IBD.
Methods
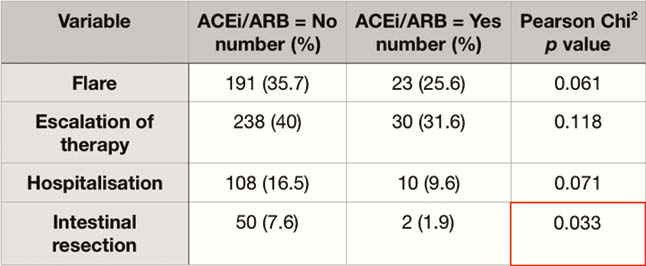
In a well-characterised cohort of IBD patients, followed up for a minimum of 2 years, baseline demographics and longitudinal disease activity were compared between patients using ACEi/ARB and those not. We reviewed case notes for flare or glucocorticosteroid use, escalation of medical therapy, hospitalisation, and intestinal resection. In univariate analyses, the χ² test was used to compare categorical variables and independent samples t-test for continuous data. A P value of <0.05 was considered statistically significant. Multivariate Cox regression analyses were expressed as hazard ratios (HR) with 95% confidence intervals (CI).
Results
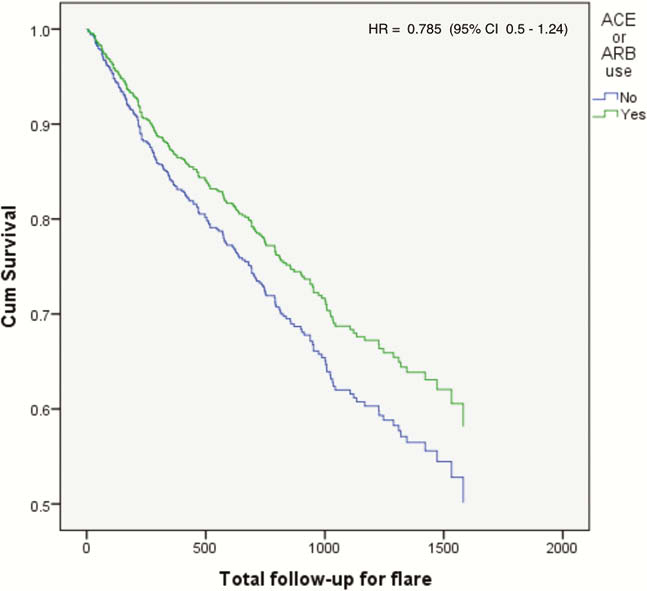
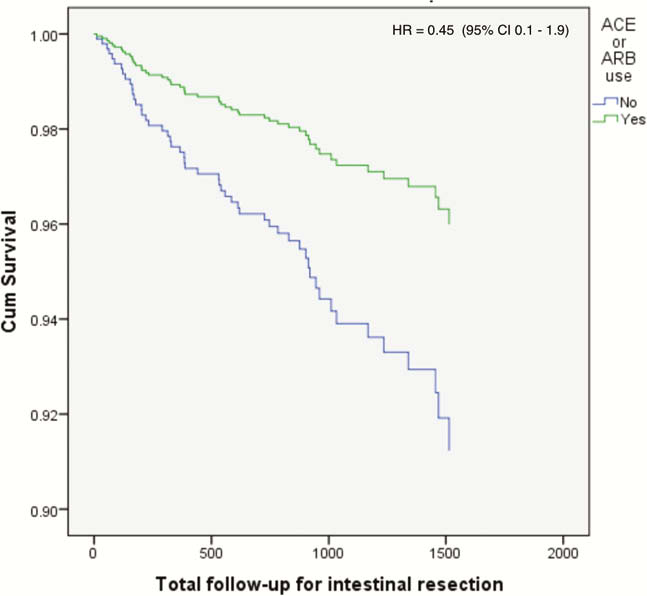
In total, 764 patients with IBD (UC = 321, CD = 443) were included. There was no significant difference in baseline demographics (sex, ethnicity, and smoking) between those with ACEi/ARB use or non-use. Mean age was higher in those taking ACEi/ARBs (60 ± 13 vs. 41 ± 16). Univariate analyses showed a trend towards improved outcomes in those using ACEi/ARB, which was significant for intestinal resection (Table 1). Following multivariate Cox regression analysis, a continued trend of improved outcomes with ACEi/ARB use was observed (Graphs 2 and 3).
 |
Conclusion
These data show a trend towards improved longitudinal disease activity outcomes in IBD patients using ACEi/ARBs. The study may be underpowered to detect a significant difference in these comparisons. Future studies performed in larger cohorts, with longer follow-up may yield significant results.
Garg M.


