P427 Exploring phenotype and treatment of inflammatory bowel disease in the elderly
Gaglani, R.(1);Balarajah, S.(1);Williams, H.(1);Hicks, L.(1);
(1)Imperial College Healthcare NHS Trust, Gastroenterology, London, United Kingdom;
Background
On a background of an ageing population, approximately 10-15% of new cases of IBD are diagnosed in patients over the age of 60.1,2 Studies show IBD in the elderly is increasing, including both the groups of patients diagnosed at a younger age, and de novo elderly IBD.
Older patients are more likely to have other co-morbidities and be concurrently prescribed other medications, which may impact the choice and timing of therapies for their disease. It is not clear if IBD in older age is different phenotypically from that in younger counterparts, and whether current management algorithms can be used safely in this cohort.
Aims of the study were to evaluate the IBD phenotype and use of therapies in the elderly (≥75 years) and younger (18-74 years) patients, and to assess for differences in adverse outcomes between both cohorts on immunosuppressants (IMs) and/or biologics.
Methods
A retrospective study was performed on 173 IBD patients at Imperial College Healthcare NHS Trust over a two-year period. 91 elderly IBD patients were compared with 82 younger patients, matched by gender and IBD subtype. Analysis included chi-squared tests with Fisher’s correction.
Results
There were 55 elderly patients and 51 younger matched patients with ulcerative colitis (UC) where no differences in disease extent, remission or surgeries were seen. There were 36 elderly patients and 31 younger matched patients with Crohn’s disease (CD). There was less ileocolonic disease in the older CD cohort compared to younger patients (27.8% versus 51.6%, p=0.046) (figure 1).
Medication use in UC was the same regardless of age. There was significantly higher use of IMs and biologics in younger patients with CD (51.6%) versus the older cohort (25%, p=0.047) (figure 2).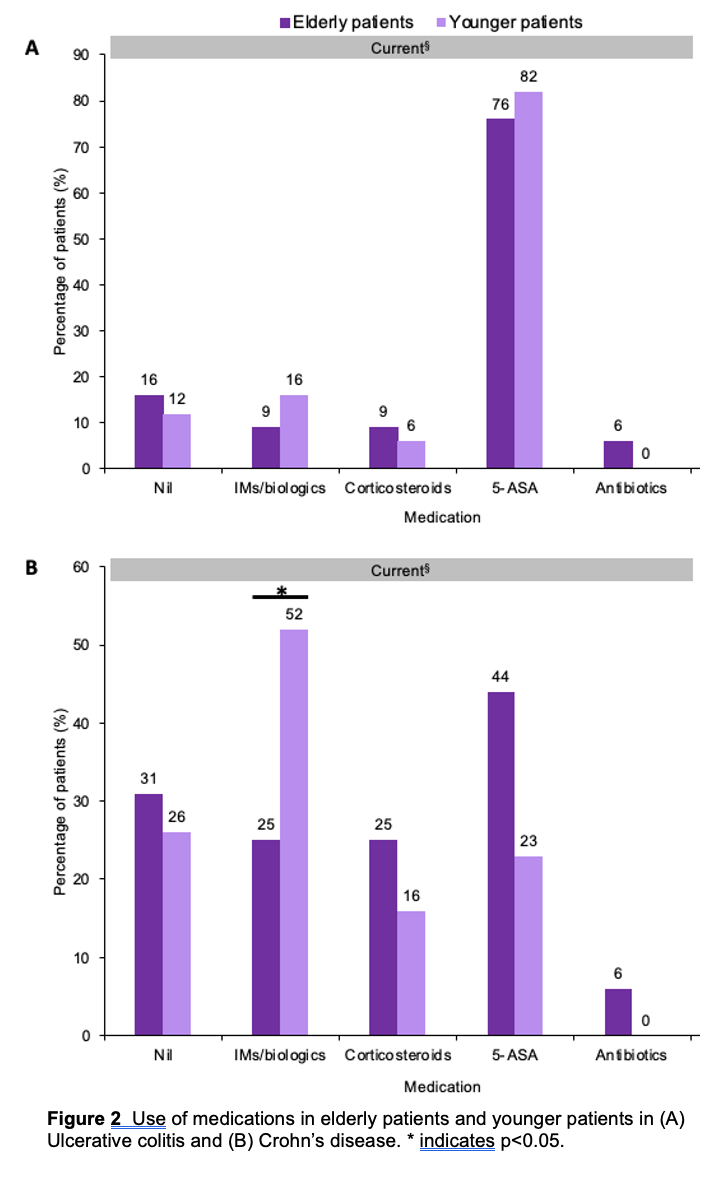
In elderly patients with CD, a significantly greater mortality was seen in patients on IMs/biologics (27.3%) than those not on these medications (8%, p=0.023) (figure 3). The rate of VTE was higher (18.2% versus 0%) in those on these treatments with a trend towards significance.
Conclusion
Overall, this retrospective study demonstrated that elderly IBD patients in this cohort appear to be mostly phenotypically similar to younger patients. However, elderly Crohn’s patients were less likely to be escalated to IMs/biologic treatments than their younger comparators. In view of the higher rate of adverse events recorded in the Crohn’s group managed with these treatments, this may be justified. Further, larger studies in the long-term outcomes of these patients are required.
References:
1. Charpentier C et al. Natural history of elderly-onset inflammatory bowel disease: a population-based cohort study. Gut. 2014;63(3),423-432


