P440 Polimedication in patients with inflammatory bowel disease: prevalence and outcomes in a retrospective unicentric series
F. Mesonero Gismero, C. Fernández, E. Sánchez-Rodríguez, A. García-García de Paredes, A. Albillos, A. López-Sanromán
Department of Gastroenterology, Hospital Universitario Ramón y Cajal, Madrid, Spain
Background
Polymedication (PM) can complicate course and management of chronic diseases, and is currently a poorly explored issue in patients with inflammatory bowel disease (IBD).
Our aims were to determine the prevalences of PM, and of inappropriate and high-risk drugs use (APINCH) in a clinical series of IBD patients, describing epidemiological factors associated with PM, and evaluating a possible association of PM with poor disease outcomes.
Methods
A retrospective observational study of a unicentric series, including patients with IBD visited at our Unit (September-October 2018). Prescriptions, demographic data, and clinical features were collected reviewing clinical files and electronic drug prescriptions. PM was defined as the simultaneous use of more than 5 drugs (Gnjidic D, J Clin Epidemiol. 2012). APINCH drugs included insulin, antibiotics, anticoagulants, chemotherapies, narcotics, and potassium supplements (Clinical Excellence Australian Commission 2017). Disease outcomes (flares, hospitalisations, surgeries), non-adherence to treatment and undertreatment were evaluated 12 months after the index visit.
Results
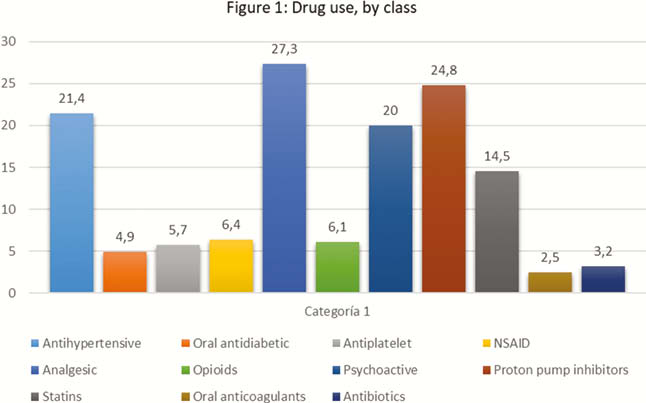
We included 407 patients (56% males, median age 48 yo, range 17–92, 60.2% Crohn′s disease, 38.8% ulcerative colitis). Chronic comorbidity was present in 54% (29% metabolic, 25.5% cardiovascular, 12.8% psychiatric), and 27% presented multiple comorbidities (≥3). Median patient number of prescriptions was 3 (r 0–15); 14.3% were on more than three drugs, and 15.7% between four and five drugs. Most frequent prescriptions are represented in Figure 1. PM was identified in 18.4% of cases, inappropriate medication in 8.8%, and high-risk drugs in 6.1% (mainly opioids). In multivariate analysis, factors significantly associated with PM were chronic comorbidity (OR 11, CI 2.3-51,2, p˂0.002), multiple comorbidities (OR 4.02, CI 1.93–8.38, p˂0.001), and age >62 years (OR 3.66, CI 1.7–7.7, p˂0.001). In univariate analysis, both undertreatment (54% vs. 16%, p˂0.01) and non-adherence (26% vs. 12%, p˂0.02) were associated with PM after 12 months. No association of PM with poor disease outcomes was found. In multivariate analysis, only undertreatment was significantly associated with PM (OR 5.9, CI 1.4–29.4, p˂0.014).
Conclusion
PM occurs in around one of the five patients with IBD, mainly in the elderly and in those with comorbidity. This scenario could interfere with appropriate IBD treatment and therapeutic success.


