P446 Plasma rich in growing factors as treatment for perianal fistulas in Crohn’s disease: unicentre experience.
Soto Sánchez, A.(1);Hernandez Camba, A.(2);Hernández, M.(1);Hernández, G.(1);Pérez Sánchez, E.(1);Barrera Gómez, M.(1);
(1)Hosp. Universitario Nuestra Señora de la Candelaria, Department of Surgery, Santa Cruz de Tenerife, Spain;(2)Hosp. Universitario Nuestra Señora de la Candelaria, Department of Gastroenterology, Santa Cruz de Tenerife, Spain
Background
Perianal Crohn’s disease (PCD) adds a significant morbidity and reduced quality of life. Complex fistulas occur in up to 20% of patients. The available treatment of PCD includes immunosuppressive drugs, antibiotics, different surgeries but are associated with high recurrence rates. A new alternative using plasma rich in growth factors (PRGF) for the treatment of complex fistulas has emerged from to achieve better healing with the minimum possible complications without affecting anal continence. This study aims to assess the feasibility, safety and efficacy of local injection of PRGF in patients with PCD.
Methods
Retrospective observational and descriptive study analyzing 6 Crohn´s Disease (CD) patients undergoing complex anal fistula sealing with PRGF from March 2019 to December 2020. All patients underwent endoanal ultrasound and 60% a pelvic magnetic resonance also. The technique consisted of locating the tract without the use of hydrogen peroxide, active curettage of the tract and closure the internal fistulous orifice (IFO) with single stitches Vicryl® 3/0. Subsequently, 50% of the PRGF-rich fraction was injected in the submucosa of the closed internal fistula orifice. The other 50% is injected in the fistulous tract. With PRGF-poor fraction a three-dimensional fibrin matrix is created and filled the previously curetted fistulous tract. We describe the results in terms of demographic variables, outcomes, surgical procedure and complications. Endpoint was fistula closure by physical examination and endoanal ultrasound.
Results
Sixty seven percent of the patients were female, mean age was 43 (26y SD). The clinical characteristics of the patients are described in table 1. All of the patients had previous abscess drainage surgery. The most frequent fistula was mid-transsphincteric type. 66.7% had seton at the time of surgery and only one patient had no medical treatment at that time. The median follow-up was 30 months. The recurrence rate was 66.7% with no differences with in age, sex, comorbidity, type of fistula, fistula location, medical treatment and whether they had a seton implanted at the time of surgery. No patient presented complications. The median follow-up was 16 months.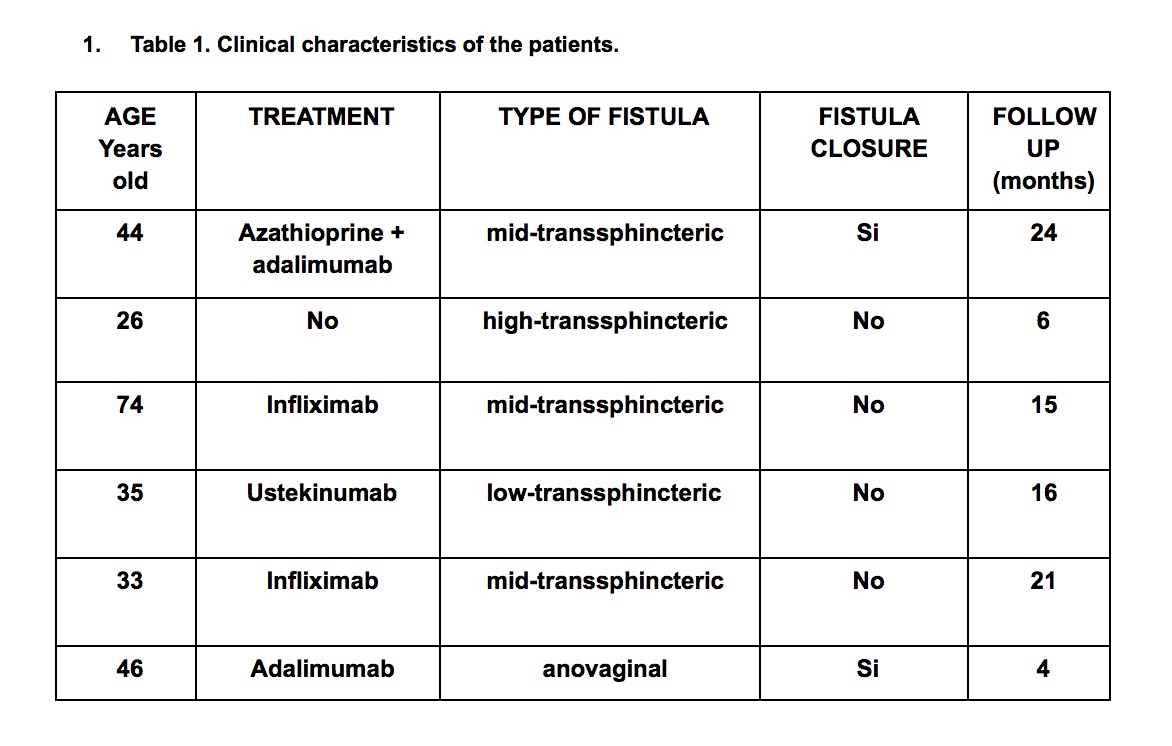
Conclusion
PRGF sealing appears to be feasible, safe and a promising option in the treatment of PCD. Further studies should be carried out to determine the real use of PRGF in PCD.


