P454 Serum oncostatin M predicts mucosal healing in Crohn’s disease patients treated with infliximab
L. Bertani1, L. Antonioli2, M. Fornili2, M. Fornai2, G. Tapete1, E. Albano1, G. Baiano Svizzero1, L. Ceccarelli3, M.G. Mumolo3, L. Baglietto2, S. Marchi1, C. Blandizzi2, F. Costa3
1Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy, 2Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy, 3Department of General Surgery and Gastroenterology - IBD Unit, Pisa University Hospital, Pisa, Italy
Background
A number of Crohn’s Disease (CD) patients fail to respond to infliximab (IFX) treatment. For this reason, the identification of a biomarker suitable to predict treatment outcome represents one of the most intriguing challenges for gastroenterologists. Oncostatin M (OSM) is a member of the interleukin 6 cytokine family, which is upregulated significantly in CD inflamed intestinal mucosa. OSM has been suggested as a promising biomarker to predict the responsiveness to anti-TNF therapy in patients with inflammatory bowel diseases. The aim of the present study was to evaluate the suitability of the evaluation of OSM serum levels as a predictive marker of treatment response to IFX.
Methods
We included CD patients treated with IFX during 2017 and 2018. All patients underwent a colonoscopy at week 54, when treatment response was evaluated in terms of mucosal healing (MH, defined as disappearance of ulcers). At baseline and after 14 weeks of treatment, OSM was evaluated by ELISA on serum samples collected before drug infusion. We assessed also faecal calprotectin (FC) at baseline and week 14. Mann-Whitney test was used to evaluate the correlation between OSM and FC levels at baseline and week 14 with MH at week 54. Spearman correlation between OSM and FC values at baseline and week 14 was computed as well. Logistic regression models to predict MH at week 54 were carried out by the Akaike Information Criterion (AIC) and Area Under the Curve (AUC).
Results
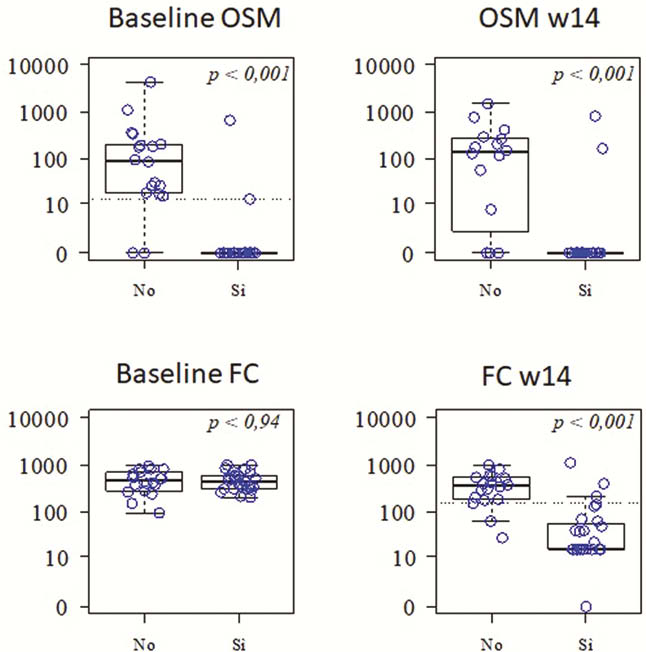
In a cohort of 45 patients (24 males) included in the study, 27 displayed MH. At baseline, OSM levels were significantly lower in treatment responders than non-responders (
Conclusion
These preliminary data suggest that OSM and FC are able to predict the outcome of treatment with IFX. Of note, at variance with FC, the predictive capability of OSM was appreciable at baseline, thus allowing to propose OSM as a promising biomarker for driving therapeutic choices in Crohn’s disease patients.


