P499 Use of an Inflammatory Bowel Disease illustrated guide as a patient education tool
Murray, J.(1);Lindsay, J.(1);
(1)Royal London Hospital- Barts Health NHS Trust- London, Department of Gastroenterology, London, United Kingdom
Background
Inflammatory bowel disease (IBD) is a lifelong condition with a major impact on QOL. Patient education and empowerment are cornerstones of high quality IBD patient care 1 and IBD clinical nurse specialists (CNS) play a key role in patient education within IBD. Multiple barriers to effective patient education exist and tools which overcome these are required. We explored IBD CNS’s opinion on (i) the barriers to effective education of patients, (ii) tools they use to overcome these barriers and (iii) the effectiveness of the use of an IBD illustrated guide.
Methods
We studied a guide developed by PostScript Medical™. An illustrative guide to Inflammatory Bowel Disease contained 20 anatomical illustrations related to IBD and its management (Figure 1). The guide and participation in the study were advertised online via UK IBD nursing networks and sent out to those who registered interest. Participants were encouraged to use the guide as frequently as possible in patient consultations. 8 weeks later an electronic survey was sent to all those who received the guide.

Figure 1. IBD multi-disciplinary team (MDT) members were involved in guide development, it can be personalised during each consultation using the attached dry wipe pen
Results
68 UK IBD CNS registered interest in the study and were sent a guide, 47 follow-up survey responses were received (response rate 69%). The top 3 reported barriers to effective patient education were complex terminology (81.63%), time limitations (81.63%) and existing patient knowledge (69.39%). The most frequent tools used to overcome these included patient information leaflets (63.27%), own drawings or sketches (57.14%) and print outs from websites (57.14%). 100% of respondents felt easily accessible visual support tools would help overcome some of these challenges. Responses on the effectiveness of the guide are shown in table 1 and 2. 100% of respondents would use the guide again in future consultations. 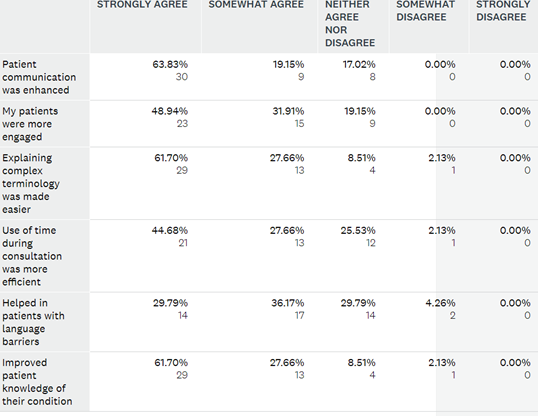
Table 1. Responses on effectiveness of guide during patient consultations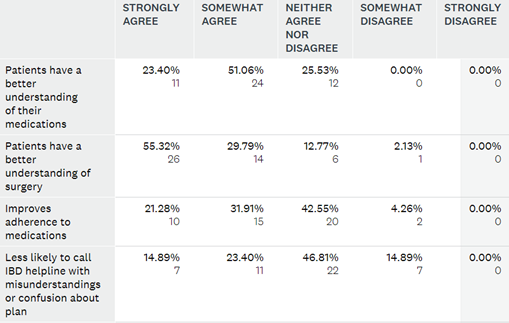
Table 2. IBD CNS perception on how guide may affect patient outcomes
Conclusion
This study identified key barriers to IBD CNS based patient education and common tools used to overcome them. It demonstrated the perceived benefit on patient understanding and engagement of using the PostScript Medical™ guide during patient consultations. This should be further explored by analysing patients’ perspective along with other members of the IBD MDT as we seek to explore tools that enhance IBD patient understanding and improve the personalised care we deliver to our patients.
References
1. Kapasi R. et al. Consensus standards of healthcare for adults and children with IBD in the UK. Frontline Gastroenterology 2020;11:178-187.


