P506 Rates of clinical remission among patients with Ulcerative Colitis from real-world clinical practice settings from Germany
Bokemeyer, B.(1);Picker, N.(2);Kromer, D.(2);Rosin, L.(3);Patel, H.(4);
(1)Gastroenterology Practice, Minden, Minden, Germany;(2)Ingress Health HWM, GmbH, Wismar, Germany;(3)Galapagos Biopharma Deutschland, GmbH, München, Germany;(4)Galapagos, Nv, Mechelen, Belgium;
Background
Patients with Ulcerative Colitis (UC) may not equally respond to advanced therapies. Therapy modifications such as dose adjustments, augmentation, and use of corticosteroids (CS) are required to achieve remission. This study aimed to examine the rates of clinical remission requiring adjustments with advanced therapies among UC patients from real-world clinical practices in Germany.
Methods
Using a retrospective chart review, patients with UC treated with an advanced therapy (adalimumab, infliximab, golimumab, vedolizumab, and tofacitinib) between 01/2017 through 09/2019 were selected from 18 outpatient gastroenterology practices across Germany. Patients with at least 12 months of data before (baseline) and after initiating an advanced therapy (Index Date) were included. Data was collected up to 24 months after index date. Clinical remission was assessed based on a partial Mayo score ≤1. Among patients with remission, therapy adjustments were assessed based on the following: Dose escalation, augmentation with conventional therapies, CS use for ≥12 weeks, or any use of CS during the maintenance phase. Time to remission was analysed using Kaplan-Meier analysis and associated factors were assessed within a multivariate Cox regression model. Patients were censored at end of the study period or if they discontinued or switched the index therapy.
Results
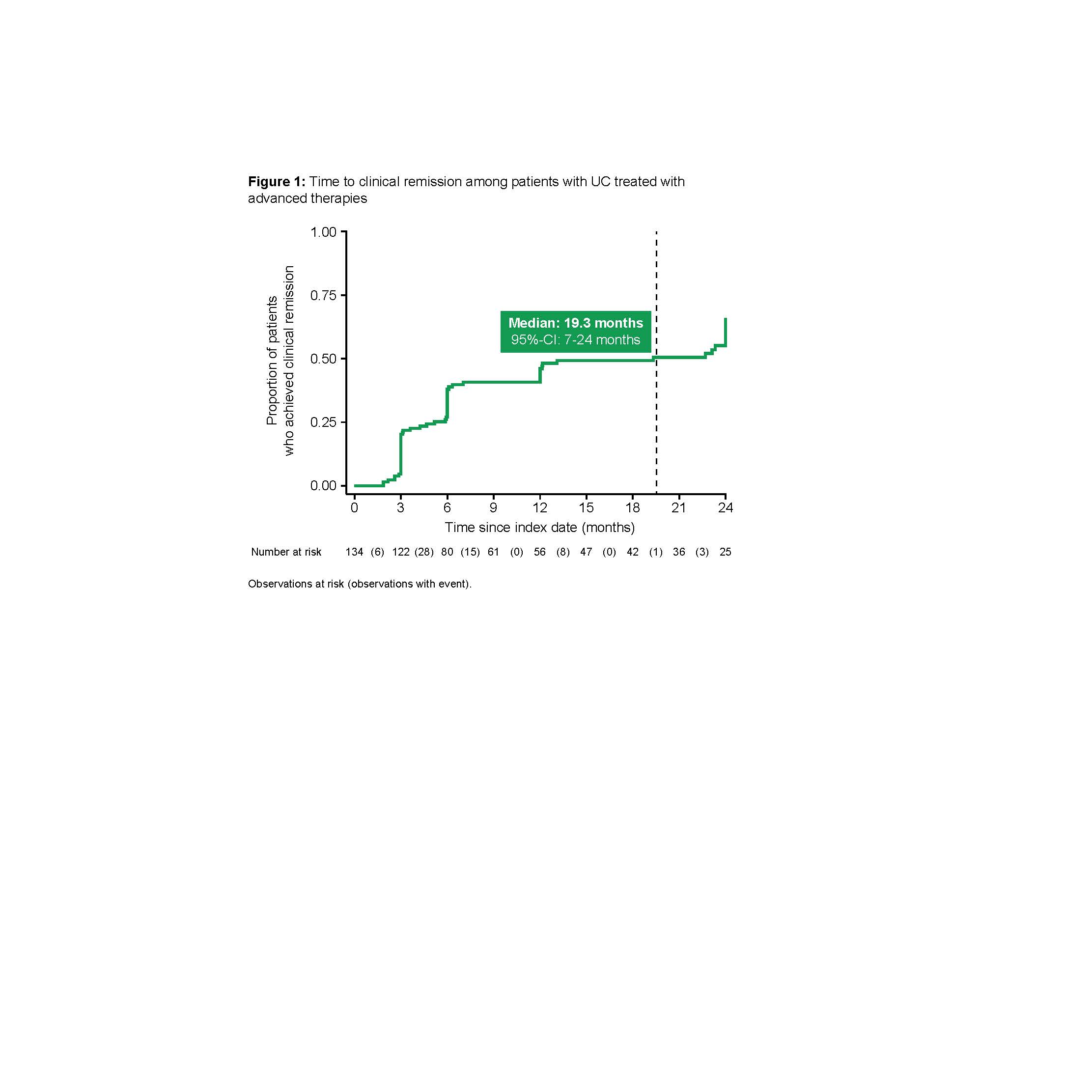
Among 149 patients included (females: 50.3%; median age: 40 years; median follow-up: 25.9 months), 75 (50.3%) received an anti-TNF agent, 48 (32.2%) vedolizumab, and 26 (17.4%) tofacitinib. Of these, 96 (64.4%) patients were biologic-naïve, and 42 patients (28.2%) were receiving concurrent CS at the index date. Within one year, remission was achieved in 49 out of 134 patients (46.1%; median time: 19.3 months [95%-CI: 7-24 months]; Figure 1). Among patients with remission at 24 months, therapy adjustments were required in 35.8% of patients. Most common adjustments included dose escalation (9.0%) and use of CS during the maintenance phase (11.9%). In an adjusted model, chances of remission were halved in biologic-experienced patients vs. naïve patients (hazard ratio [HR]: 0.49; p<0.05), while patients with concurrent use of conventional therapy at baseline were associated with a higher chance of achieving remission (HR: 1.82; p<0.05).
Conclusion
Less than half of UC patients treated with advanced therapies in Germany achieved clinical remission after one year. More than half of the patients required 1.5 years to achieve clinical remission. Among those who achieved remission within two years, one third required additional therapy modifications. More effective therapies are needed to achieve earlier and better outcomes among patients with UC in Germany.


