P507 Need for surgery in patients with ulcerative colitis in the era of biologic therapy.
Zamora Olaya, J.M.(1);Aparicio-Serrano, A.(1);Gómez Pérez, A.(1);Ortiz Chimbo, D.S.(1);Rodríguez Tirado, M.I.(1);Soto Escribano, P.(1);Marín Pedrosa, S.(1);Iglesias Flores, E.(1);Benítez, J.M.(1);
(1)Reina Sofía University Hospital, Gastroenterology and Hepatology, Córdoba, Spain; IMIBIC
Background
The aim of the present study is to evaluate the impact of anti-TNF drugs on the need for surgery among patients with ulcerative colitis (UC). Secondary objectives: to compare needs for medical treatment before surgery, indications for surgery and surgery-free survival.
Methods
Observational, retrospective and single-center study that includes patients with UC who have required surgery for inflammatory bowel disease (IBD). Two cohorts of UC patients were analyzed: cohort-1 (pre-antiTNF) with a diagnosis of UC between 1995-2000, and cohort-2 (post-antiTNF) diagnosed after the approval of anti-TNF between 2010-2015. Patients were followed up to the event (surgery) or at least five years since UC diagnosis. Demographic variables related to UC and surgery were collected. Kaplan-Meier curves were performed to compare the surgery-free survival in both cohorts. The ENEIDA registry was used to identify the patients.
Results
A total of 32 patients underwent surgery were included (18 in cohort 1 and 14 in cohort 2). The mean age at UC diagnosis was significantly lower in cohort 1 (31.3 vs 46.4 years, p=0.015), and the proportion of smoking patients was higher in cohort 1 (27.8% vs 0%, p=0.053). There were no differences between the two cohorts in the extent of UC and extraintestinal manifestations. Surgery rates were 3.7% in cohort-1 and 4.7% in cohort-2. Overall, there were no differences in colectomy rates in both cohorts (Figure 1). However, the median time from UC diagnosis to surgery was significantly longer in cohort-2 (21 vs. 1 months, p<0.05) (Figure 2). Regarding the surgery timing, the proportion of urgent surgery was higher in cohort-1 (61% vs 43%, ns); while in cohort-2, scheduled surgery predominated (50% vs 18%, ns). In the subgroup of patients who underwent scheduled surgery, the surgery free time was significantly longer in cohort-2: 67 vs 12 months (p=0.01) (Figure 3). Regarding surgical indications, cohort-1: 78% acute severe colitis or acute complications and 22% refractory to medical therapy; cohort-2: 43% Acute Severe Colitis/complications. A high proportion of patients in both cohorts required ostomy (temporary or definitive). Pre-surgery medical treatment needs cohort-1 vs cohort-2: steroids (100% vs 71%, p=0.028), immunosuppressants (5.6% vs 57%, p=0.002).
Figure 1. Surgery -free survival at 5-years follow-up.
Figure 2. Kaplan-Meier curves of time from UC diagnosis to surgery.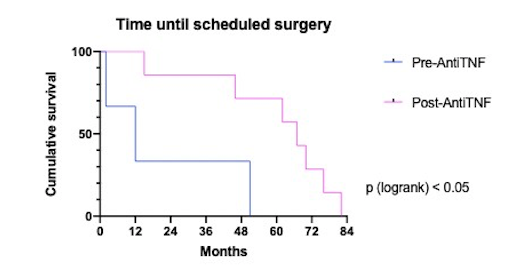
Figure 3. Kaplan-Meier curves of time until scheduled surgery.
Conclusion
Surgery rates in UC patients remain stable in the post-antiTNF era. However, the arrival of antiTNF drugs allows a longer surgery-free survival, lower preoperative steroids requirements and less need for urgent surgery.


