P546 Ileal ulcer size significantly impacts the ability to achieve endoscopic remission: a post-hoc analysis from the SONIC trial
N. Narula1, E. Wong1, A. Achuthan1, P. Dulai2, J.F. Colombel3, J.K. Marshall1, M. Ferrante4, W. Reinisch5
1Department of Gastroenterology, McMaster University, Hamilton, Canada, 2Department of Gastroenterology, University of California San Diego, San Diego, USA, 3Department of Gastroenterology, Mount Sinai Medical Center, New York, USA, 4Department of Gastroenterology and Hepatology, University Hospitals Leuven, Leuven, Belgium, 5Division of Gastroenterology and Hepatology, Department of Internal Medicine III, Medical University of Vienna, Vienna, Austria
Background
Endoscopic remission (ER) is an important target of treatment for Crohn’s disease (CD). However, it is unclear how individual baseline endoscopic characteristics impact the ability to achieve ER. We aimed to determine endoscopic prognostic factors that influence the likelihood of achieving ER in CD.
Methods
This was a post-hoc analysis of SONIC (NCT00094458; YODA #2019–3980), where data from 172 patients who had endoscopic scores at baseline and at week 26 were evaluated. Individual components of the Crohn’s Disease Endoscopic Index of Severity (CDEIS) and the Simple Endoscopic Score for Crohn’s disease (SES-CD) indices were used to evaluate the impact of baseline ulcer depth (CDEIS) and size (SES-CD) on likelihood of achieving ER at week 26. Ileum and colon segments were evaluated separately. Multivariate logistic regression models were used to evaluate the relationship between baseline endoscopic findings and achievement of ER in each segment at week 26, after accounting for known confounders including disease duration and treatment allocation. Results are presented as odds ratios (OR) with 95% confidence intervals (CI).
Results
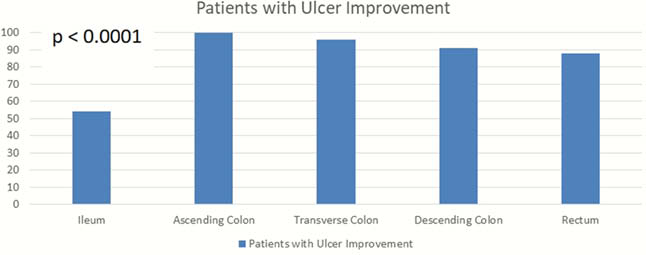
The rate of ulcer improvement in the ileum was significantly lower than rates of healing throughout the colon (
Conclusion
Ulcer size and depth, but not the overall degree of endoscopic inflammation, seem to impact likelihood of achieving week 26 ER. ER may be more difficult to achieve for patients with larger and deep ulcers in the ileum. These findings may have implications for recruitment into clinical trials and would support the importance of balancing these prognostic factors in trial arms. Further prospective data are needed to validate these findings.


