P564 Psychological acceptance of surgery in patients with inflammatory bowel disease undergoing intestinal resection
Y. Hirano1,2, M. Itabashi3, T. Saito4, K. Uchida5, M. Inoue5, A. Katsuhiro2, H. Atsuhiro1, K. Araki1, Y. Nishikawa1, M. Tatsuno1, K. Hideaki1, K. Reiko1
1Inflammatory Bowel Disease Centre, Yokohama City University Medical Centre, Yokohama, Japan, 2Division of Gastroenterology, National Centre for Child Health and Development, Tokyo, Japan, 3Department of Surgery Institute of Gastroenterology, Tokyo Women’s Medical University, Tokyo, Japan, 4Department of Pediatric Surgery, Chiba University Graduate School of Medicine,Chiba, Japan, 5Department of Gastrointestinal and Pediatric Surgery, Mie University Graduate School of Medicine, Mie, Japan
Background
To decision to undergo surgical intestinal resection is among the most difficult that patients with inflammatory bowel disease (IBD) may be required to make during the disease course. Although the clinical outcomes and QoL after intestinal resection are well established, few studies have focused on psychological acceptance of the surgery, that is, how patients feel about the results of intestinal resection. The aim of this study was therefore to evaluate psychological acceptance of the surgical outcome in patients undergoing intestinal resection.
Methods
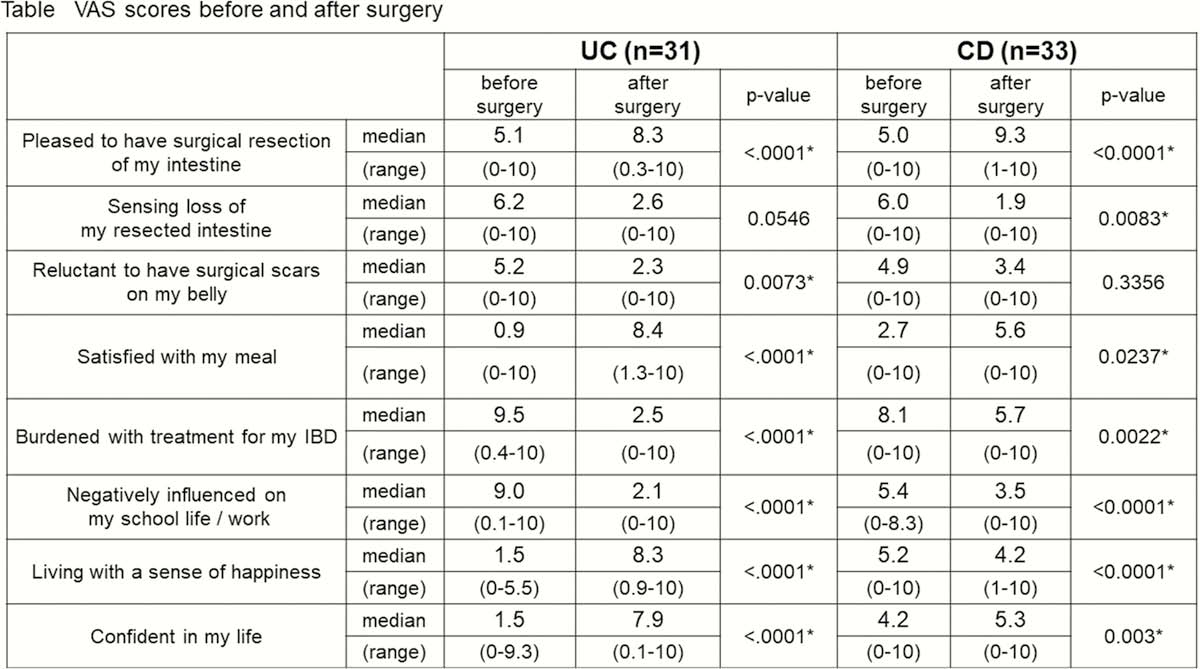
We administered a cross-sectional questionnaire survey to patients at five IBD centres in Japan who had undergone intestinal resection at least 1 month before the survey. Patients were asked to complete a visual analogue scale (VAS) questionnaire, consisting of 20 questions related to surgical acceptance and concerns related to IBD (body image, burden of treatment, interpersonal relationships), before and after surgery. The VAS scores before surgery were described by the patient looking back on recollection. Pre- and post-surgical VAS scores were compared using a Wilcoxon’s rank-sum test.
Results
A total of 64 patients participated in this study (median age at surgery 37.9 (range 12–67) years, median years after surgery 5.0 (range 0.1–21) years). The VAS scores before and after surgery were summarised in the figure. The score for ‘pleased to have surgical resection of my intestine’ improved significantly after the surgery in both UC and CD (
Conclusion
Our findings indicate that surgical intestinal resection outcomes were psychologically well accepted by most IBD patients.


