P581 Early biological therapy within the first 12 months after diagnosis leads to higher clinical, endoscopic, and transmural remission in Crohn’s disease: European multicentre study with a propensity-score matched analysis
Revés, J.(1)*;Fernandez-Clotet, A.(2);Ordás, I.(2);Buisson, A.(3);Ellul, P.(4);Elorza, A.(5);Aduna, M.(6);Rodríguez-Lago, I.(5);Freire, G.(7);Sousa, P.(7);Primitivo, A.(7);Delgado, I.(7);Sousa Lajas, I.(8);Raimundo, A.(8);Bettencourt, P.(8,9);Rimola, J.(10);Torres, J.(1,11);
(1)Hospital Beatriz Ângelo, Gastroenterology Department, Loures, Portugal;(2)Hospital Clínic de Barcelona- Institut d’Investigacions Biomèdiques August Pi i Sunyer IDIBAPS- and CIBEREHD, Department of Gastroenterology, Barcelona, Spain;(3)Université Clermont Auvergne- Inserm- CHU Clermont-Ferrand, Department of Gastroenterology, Clermont-Ferrand, France;(4)Mater Dei Hospital, Division of Gastroenterology, Msida, Malta;(5)Hospital Universitario de Galdakao, Department of Gastroenterology, Galdakao, Spain;(6)OSATEK-hospital de Galdakao, Department of Radiology, Galdakao, Spain;(7)Hospital Beatriz Ângelo, Department of Radiology, Loures, Portugal;(8)Universidade Católica Portuguesa, Faculty of Medicine, Rio de Mouro, Portugal;(9)Universidade Católica Portuguesa, Centre for Interdisciplinary Research in Health, Lisbon, Portugal;(10)Hospital Clínic de Barcelona- IDIBAPS, Department of Radiology, Barcelona, Spain;(11)University of Lisbon, Faculty of Medicine, Lisbon, Portugal;
Background
Transmural healing (TH) is emerging as a potential treatment target for Crohn´s Disease (CD). While post-hoc analyses of RCTs and observational studies have shown that early introduction of biological therapy leads to higher rates of clinical (CR) and endoscopic remission (ER), no data is available for TH. Our goal was to assess the impact of early biologic introduction (defined as <12 months since diagnosis) in CR, ER, and TH rates.
Methods
Multicentre retrospective study including 5 European centres. Patients with CD with a baseline (±3 months) either computed tomography enterography (CTE) or magnetic resonance enterography (MRE) with signs of active disease before starting biologics were included. We assessed CR (PRO2<8), ER (SES-CD<3 and no ulcers), and TH (complete normalization of MRE) at 12±3 months following the introduction of biologics. All radiological examinations were read locally after a consensus meeting to list and define clinically relevant lesions and outcomes. Multivariate logistic regression with propensity-score matching also adjusted for previous biologic use was conducted (propensity-score covariates: gender, age at diagnosis, disease location, disease behavior, perianal disease, extra-intestinal manifestations, smoking history, and previous surgery).
Results
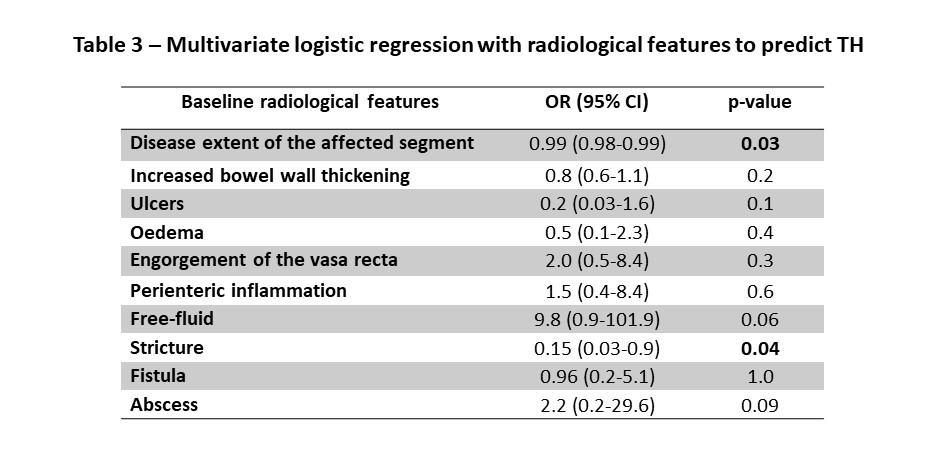
We included 168 patients (51% females), with a median age at diagnosis of 25 years old (IQR 19-34). Median follow-up time after treatment initiation was 73 (IQR 42-98) months and median disease duration was 120 (IQR 76-237) months. Most patients (93%) had ileal involvement (L1 or L3) and an inflammatory phenotype (50%). Overall, 79% were bio naïve and of those 46% were started on early biological treatment. Most patients were started on anti-TNF (89%), 10% on ustekinumab, and 1% on vedolizumab; 58% were on combination therapy (table 1). CR was achieved in 76% (119/157), ER in 52% (64/124), and TH in 32% (30/95). In the multivariate logistic regression model, early initiation of biological treatment was significantly associated with increased probability of achieving CR (OR 4.3, 95%CI 1.6-11.5, p=0.003), ER (OR 2.9, 95%CI 1.2-7.1, p=0.02) and TH (OR 2.7, 95%CI 1.002-7.1, p=0.049). The presence of a stricture in endoscopy was a negative independent factor to predict ER (table 2) and the presence of a stricture and extensive disease in cross-sectional imaging were negative independent factors to predict TH (table 3).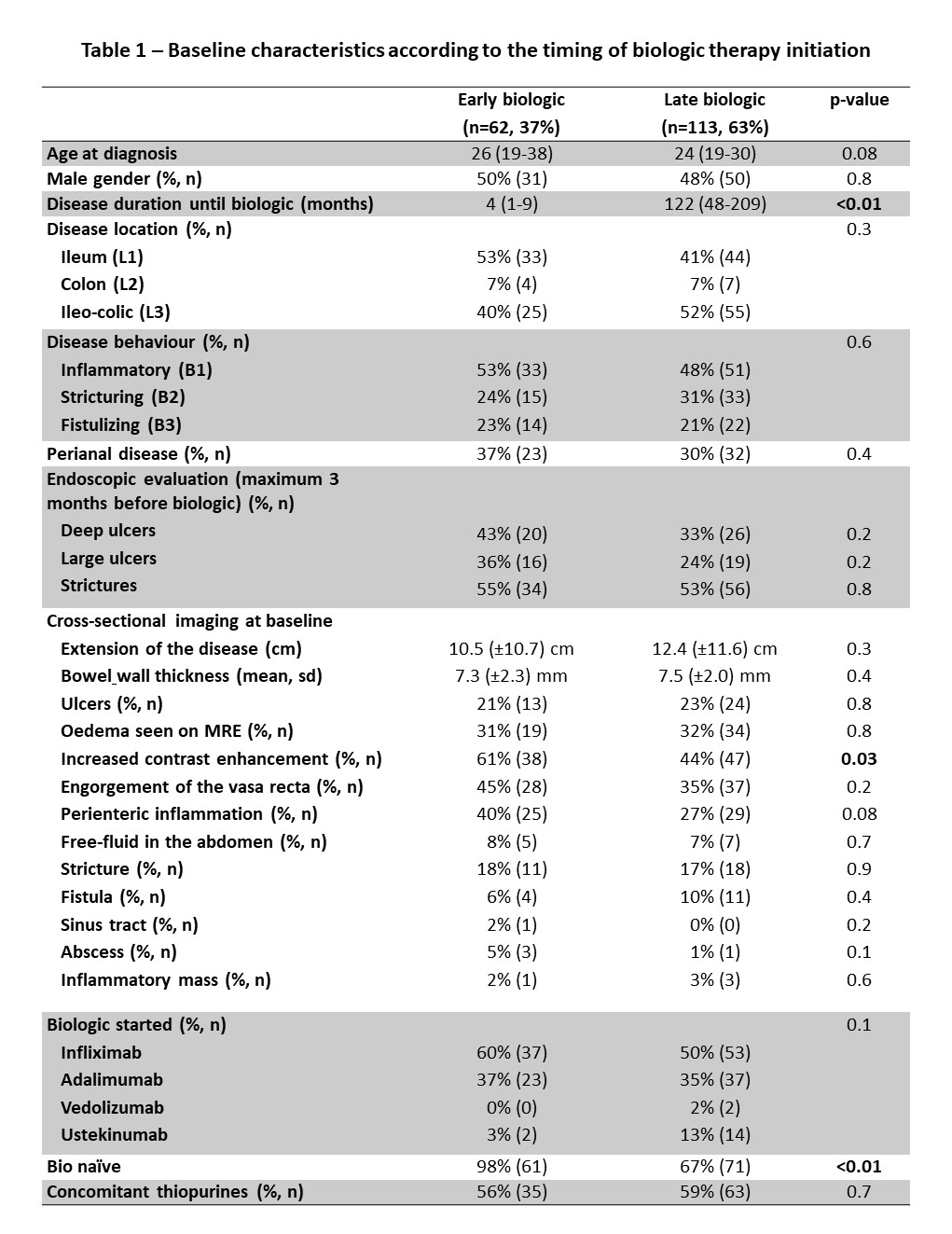

Conclusion
Introducing biological treatment within the first 12 months after diagnosis was associated with an increased probability of achieving CR, ER, and TH. The presence of a stricture both in endoscopy and in cross-sectional imaging and the radiological extension of the disease may limit the achievement of ER and TH, respectively.


