P604 Evaluation of management heterogeneity and complications of Crohn’s disease in Catalonia. A population quality care study
Brunet, E.(1);Melcarne, L.(1);Llovet, L.(1);Vela, E.(2);Cleries, M.(2);Pontes, C.(3,4);Garcia-Iglesias, P.(1,5);Albert, V.(1,5,6);Calvet, X.(1,5,6);
(1)Hospital Parc Taulí, Aparell digestiu, Sabadell, Spain;(2)Generalitat de Catalunya, Unitat d’Informació i Coneixement. Servei Català de la Salut, Barcelona, Spain;(3)Generalitat de Catalunya, Àrea del Medicament. Servei Català de la Salut, Barcelona, Spain;(4)Universitat Autònoma de Barcelona., Departament de Farmacologia- de terapéutica i de Toxicologia., Bellaterra, Spain;(5)Instituto de Salud Carlos III., CIBERehd, Madrid, Spain;(6)Universitat Autònoma de Barcelona, Departament de Medicina, Barcelona, Spain
Background
Heterogeneity in the treatment of a disease is a marker of suboptimal quality of care. Recent studies suggest that there is a marked heterogeneity in the management of inflammatory bowel disease.
The aim of this study is to evaluate the heterogeneity in the treatment used and the outcomes (rate of hospitalization and surgery) for Crohn’s disease (CD) in the different health areas of Catalonia.
Methods
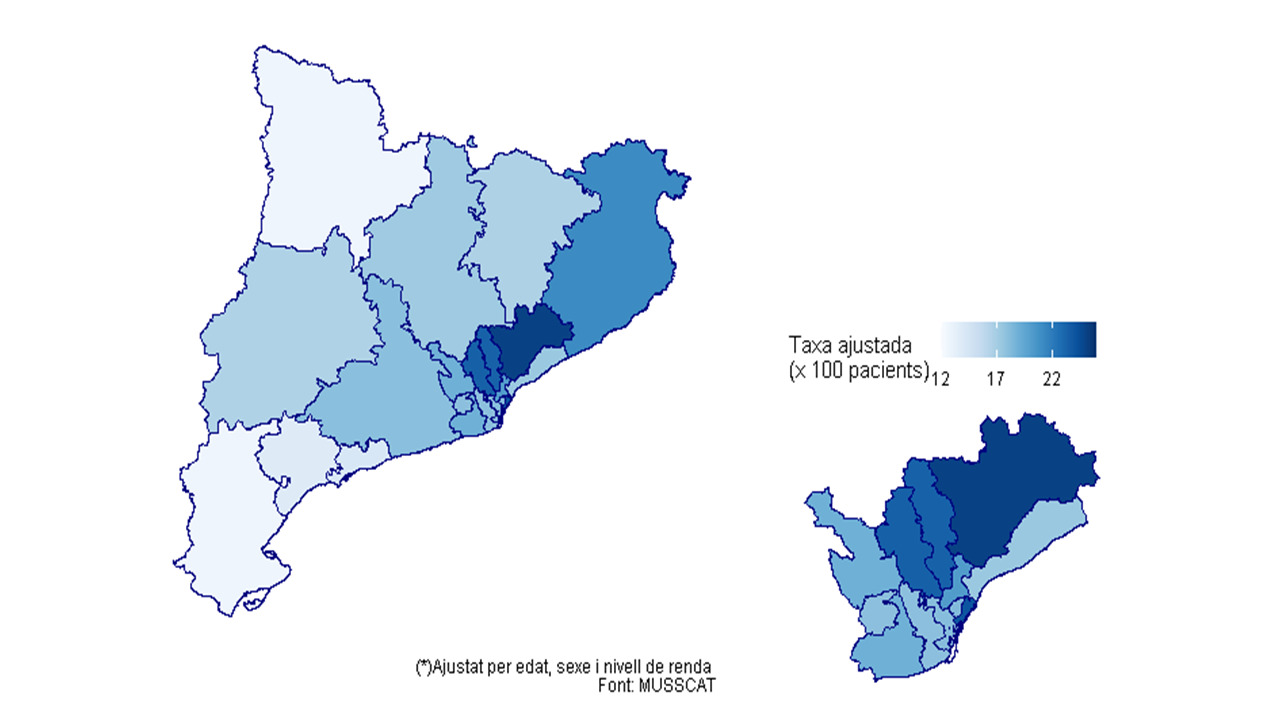
All patients with CD included in the Catalan Health Surveillance System (CHSS) including data on more than 7 million individuals from 2011 to 2017 were identified using with the ICD-9-CM codes. The different Catalonian health areas were grouped into 19 groups according to the reference hospital (figure 1). Exposures to different treatments were retrieved from the electronic dispensation records.
Data on hospitalizations and surgeries were also extracted from the CHSS according to ICD-9-CM codes. Treatment used rates (systemic corticosteroids, non-biological and biological immunosuppressant) and outcome rates (hospitalization and surgery) were calculated.
Results
The use of systemic corticosteroids presented a decreasing trend over the study period, with an average rate of use of the total number of patients in the different territories between 10% and 16% (figure 2). The use of non-biological immunosuppressant treatment has remained stable, with an average rate of use ranging from 20% to 40% (figure 3). On the other hand, the use of biological immunosuppressant treatment increased, with an average rate of use in the different territories ranging from 10 to 22% (figure 4).
Hospitalizations for any reason showed an increasing trend between 2011-2017 with an average rate between 19% and 30% per year depending on the area. Contrarily, hospitalizations for CD presented a decreasing trend, with an average rate between 5% and 10% per year.
Surgical treatment (both resections and ostomies) remained stable over time. Rates per year were between 1% and 2%.

Conclusion
In this population study we appreciated an important heterogeneity in the use of non-biological and biological immunosuppressant treatments, identifying use rates of almost the double in some of the areas. There is also a remarkable variability in the rate of hospitalizations for CD between certain areas of Catalan territory.


