P624 Investigating the symptom burden among European patients with moderate-to-severe Crohn’s disease using a real-world survey
BurischPhD, J.(1)*;Hart, A.(2);Sturm, A.(3);Knight, H.(4);Rudolph, C.(5);Meadows, R.(4);Oortwijn, A.(5);Weatherby, S.(4);Rolph, R.(6);Dawod, F.(4);Armuzzi, A.(7);
(1)Hvidovre University Hospital, Department of Gastroenterology, Hvidovre, Denmark;(2)St Mark’s Hospital, IBD Unit, Harrow, United Kingdom;(3)German Red Cross Hospital Berlin, Department of Internal Medicine - Gastroenterology, Berlin, Germany;(4)Adelphi Real World, Adelphi Real World, Bollington, United Kingdom;(5)Galapagos NV, Medical Affairs Department, Leiden, The Netherlands;(6)Galapagos NV, Medical Affairs Department, Mechelen, Belgium;(7)IRCCS Humanitas Research Hospital, IBD Center, Milan, Italy;
Background
Despite treatment, patients with Crohn’s disease (CD) experience symptoms that affect their health-related quality of life (HRQoL). Understanding how CD affects HRQoL reveals valuable insight into disease impact. We aimed to examine the disease burden in patients with moderate-to-severe CD in remission vs not in remission using real-world, gastroenterologist (GE)- and patient-reported data.
Methods
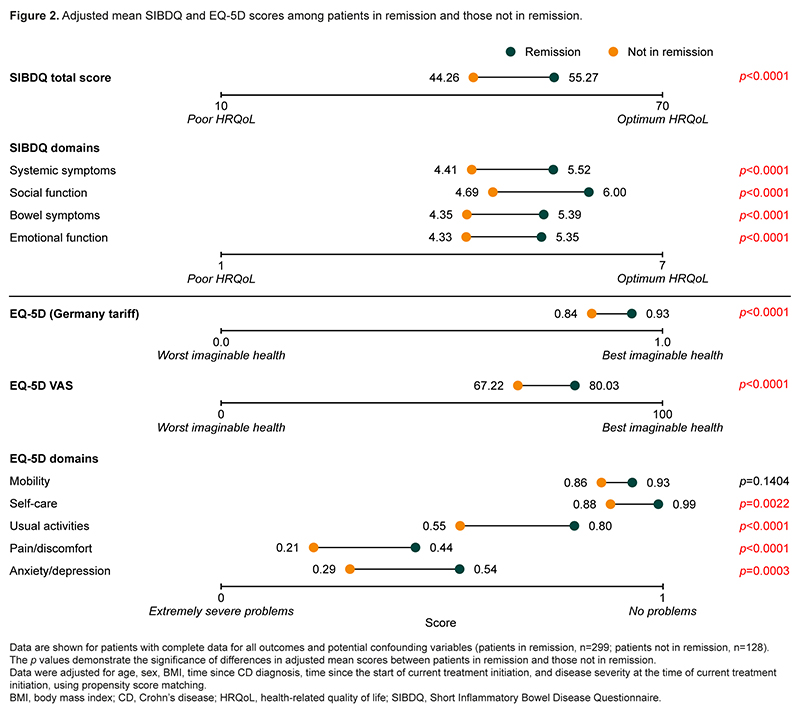
Data were drawn from the Adelphi Inflammatory Bowel Disease (IBD) Disease Specific Programme,1 a point-in-time survey conducted in France, Germany, Italy and Spain from October 2020 to March 2021. GEs collected data from the next 5–8 consecutive patients (≥18 years old, not involved in clinical trials) with a CD diagnosis who they saw in clinical practice. GEs reported patient demographics, clinical characteristics (including remission status) and treatment history. Patients completed questionnaires on their treatment satisfaction, symptoms and HRQoL (Short Inflammatory Bowel Disease Questionnaire [SIBDQ] and EQ-5D scores). Scores were compared among patients in remission vs not in remission using propensity score matching (PSM).
Results
Overall, 133 GEs reported on 538 patients with CD (Table 1). Overall, 66.0% of patients were employed, and of those not working, 24.3% were not working due to CD. Most patients (70.9%) had received ≥2 lines of treatment and 43.3% of patients were receiving a tumour necrosis factor (TNF) inhibitor. Of 427 patients from whom complete data were available and were therefore included in PSM analyses, 70.0% (n=299) were in remission. Although patients in remission were generally less likely than those not in remission to experience CD symptoms, they were still moderately likely to experience symptoms such as fatigue/tiredness and abdominal pain (Figure 1). Similarly, whilst patients in remission had better mean SIBDQ and EQ-5D scores than those not in remission, their scores still indicated diminished HRQoL (Figure 2). Of patients for whom symptom data were provided, 39.2% were either not satisfied with their current treatment or believed that better disease control could be achieved. A higher proportion of patients who were dissatisfied with their treatment reported residual symptoms than those who were satisfied, especially abdominal pain, non-bloody diarrhoea and fatigue/tiredness (Figure 3). Characteristics of patients in remission with mucosal healing were similar regardless of whether remission was confirmed by endoscopy.


Conclusion
A substantial proportion of patients with CD, even those in remission, experience high symptom burden and diminished HRQoL despite treatment. There is a need for therapies that provide more comprehensive disease control.
1. Anderson P et al. Curr Med Res Opin 2008:24;3063–72.


