P629 Evolution of disease phenotype, time to biological therapy and medium-, long-term surgery rates in Crohn’s disease patients in Western Hungary – a population-based study between 2007–2018, data from the Veszprem county cohort
Gonczi, L.(1);Lakatos, L.(2);Golovics, P.(3);Pandur, T.(4);David, G.(2);Erdelyi, Z.(2);Szita, I.(2);LakatosPhD, P.L.(1,5);
(1)Semmelweis University, Department of Medicine and Oncology, Budapest, Hungary;(2)Ferenc Csolnoky Hospital, Department of Gastroenterology, Veszprem, Hungary;(3)Hungarian Defence Forces- Medical Centre, Department of Gastroenterology, Budapest, Hungary;(4)Grof Esterhazy Hospital, Department of Gastroenterology, Papa, Hungary;(5)McGill University Health Centre, Department of Gastroenterology, Montreal, Canada;
Background
The number of prospective population-based studies evaluating the natural disease course and surgical outcomes of Crohn’s disease(CD) are still limited from Eastern Europe. The present study is a continuation of the Veszprem IBD population-based cohort with a follow-up of the incidence and disease course of IBD since 1977. Our aim was to evaluate disease course by examining progression in disease phenotype, time to biological therapy and surgery rates in a prospective population-based database from Veszprem Province, including incident CD patients diagnosed between January1,2007 and December31,2018.
Methods
Data of 421 incident CD patients were analyzed(male/female:237/184; median age at diagnosis:29 years(y)[IQR: 21-42]). Both in-hospital and outpatient records were collected and comprehensively reviewed at diagnosis and during clinical follow-up. The mean length of follow-up was 8.53y(SD: 3.3). Probability of medium-, long-term change in disease course and surgical outcomes were analyzed.
Results
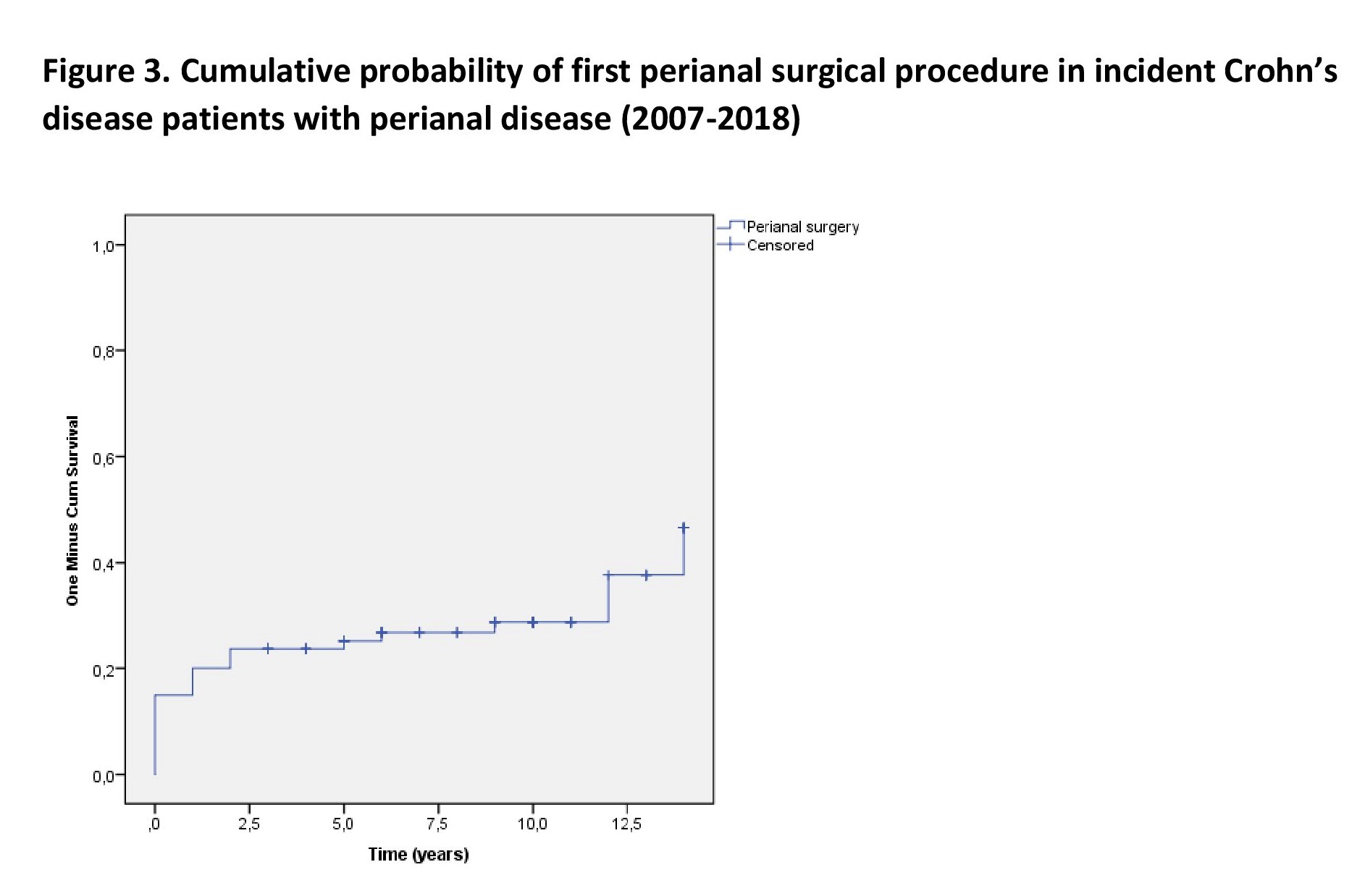
Disease location was ileal(L1), colonic(L2) in and ileo-colonic(L3) in 29.7%/24.5%/45.8% of patients at diagnosis. At the end of follow-up(8.53y), disease location was 27.1%/22.8%/50.1%(L1/L2/L3). The proportion of patients with upper gastrointestinal manifestation remained stable(7.6% and 8.1%), while perianal disease increased from 13.5% to 19% by the end of follow-up. Disease behavior at diagnosis was luminal(B1) in 62.5% of the patients. The probability of disease behavior progression from luminal into stenosing or penetrating phenotype was 11.9%(SE:1.7) at 3 years, 13.2%(SE:1.7) at 5 years and 17.6%(SE:1.7) at 10 years.Figure 1. The Probability of receiving biological therapy after diagnosis was 20.9%(SE:2.0) at 5 years and 28.8%(SE:2.0) at 10 years in this cohort. Overall resective surgery rate was 29.5% in the total population, while perianal surgery rate was 31.3% in patients with perianal disease at the end of follow-up. The probability of resective surgery was 20.7%(SE:2.0) at 1 year, 26.1%(SE:2.2) at 5 years and 30.7%(SE:2.4) at 10 years.Figure 2. For the probability of first perianal surgery among patients with perianal disease see Figure 3.


Conclusion
The probability of progression in disease behavior was lower compared to data from previous decades and similar to results from recent pan-European population-based data.(Burisch 2018, JCC). One-year surgery rates after diagnosis were considerably higher compared to previous data from our cohort or compared to Western and Northern European centers.(Lakatos 2011, IBD). Medium-term(5y) surgery rates were similar(~20%) compared to recent Hungarian and European data, while long-term(10y) rates decreased compared to data from previous decades.(Lakatos 2011,IBD; Lakatos 2012,AJG).


