P639 Outcomes of a clinical psychology intervention in a UK IBD service
F. Eldridge DClin Psyc, K. Strongili, M. Parkes, T. Raine
Addenbrooke’s Hospital, Dept of Gastroenterology, Cambridge, UK
Background
Patients with IBD experience significant psychological distress. A variety of interventions to ameliorate this distress have been studied. However, to date, no European study has assessed the impact on patients of a clinical psychologist embedded within the IBD team. Clinical psychology is uniquely characterised by its use of a patient/therapist collaborative formulation to guide and select from a variety of evidenced-based psychological therapeutic treatment options. Such an approach is likely to be particularly beneficial for patients with IBD who may present with a wide range of needs from adjustment at diagnosis to coping with symptoms, adhering to treatment protocols and managing an on-going relationship with a medical team.
Methods
A novel clinical psychology service was established within an existing IBD service at a large UK tertiary centre. Patients were referred either by a gastroenterologist, IBD nurse, or dietician using real-world clinical selection (clinical judgement rather than screening/threshold methods). Patients could also self-refer to the service. After an assessment with the clinical psychologist, patients were assigned as either accepted for intervention, referred to other mental health services or did not require intervention. Intervention involved a range of therapeutic modalities delivered by a clinician with considerable experience of working with long-term physical health conditions.
Results
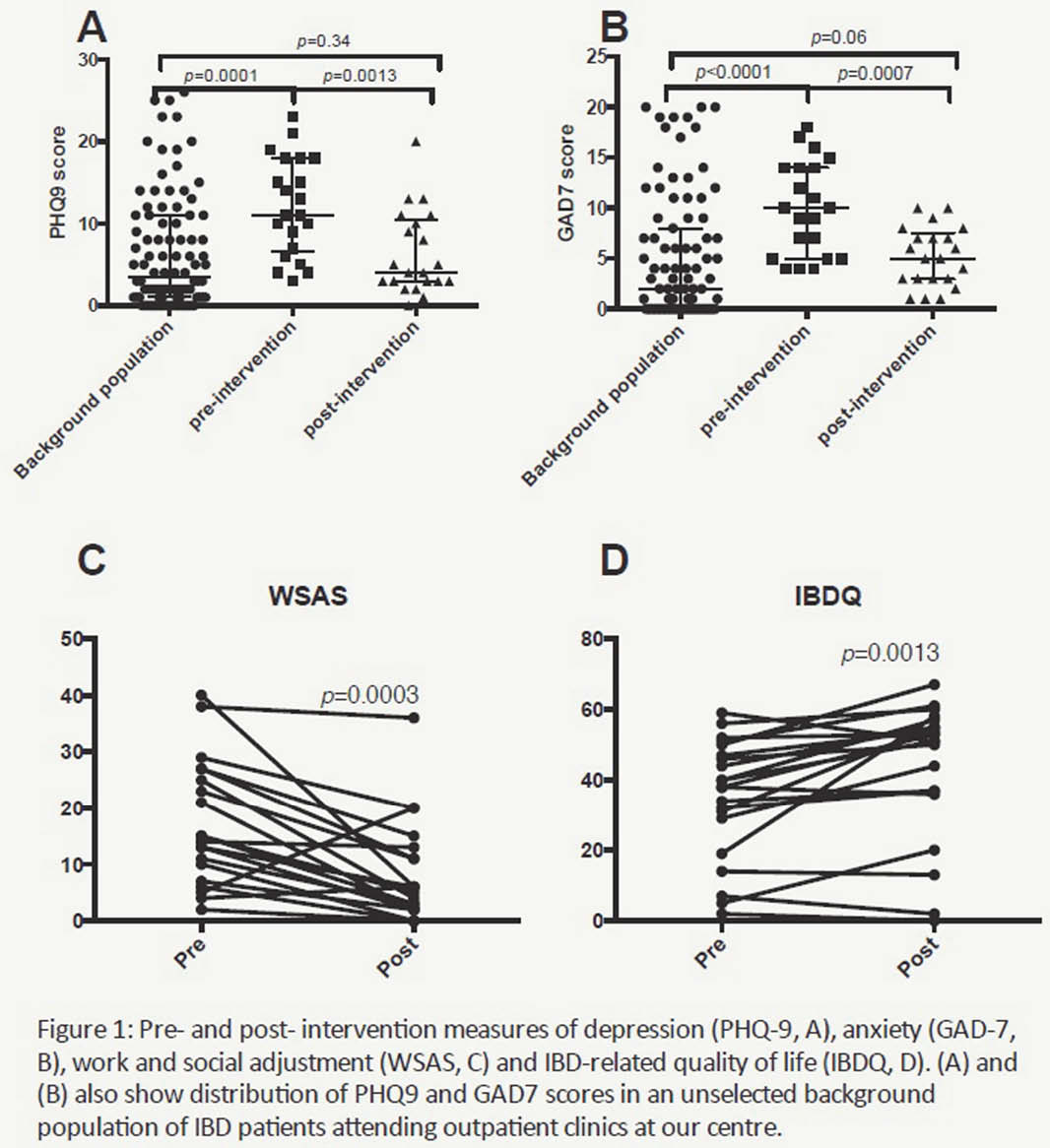
Of 42 patients referred, 25 (60%) were accepted for intervention, with completion data currently available for 21. Measures of depression, anxiety, work and social adjustment and health-related quality of life were captured for these patients pre-, during and post-intervention, as well as for 93 unselected patients with IBD attending outpatient clinics. Patients selected for intervention recorded moderate to severe scores across these domains that differed significantly from the background population. Post-intervention, patients showed highly statistically significant improvement across all domains with scores that did not differ from the background.
Conclusion
Real-world clinical selection methods appear adequate in identifying patients with greater psychological need than the baseline population. Although limited by our current small sample size, our results suggest that a clinical psychology intervention, embedded within the IBD team, can reduce patient psychological distress in IBD across a range of outcomes.


