P640 Incidence, prevalence, disease phenotype and maximal therapeutic step in Crohn’s disease patients in Western Hungary – a population-based study between 2007–2018, data from the Veszprem county cohort
Lakatos, L.(1);Gonczi, L.(2);Golovics, P.(3);Pandur, T.(4);David, G.(1);Erdelyi, Z.(1);Szita, I.(1);LakatosPhD, P.L.(2,5);
(1)Ferenc Csolnoky Hospital, Department of Gastroenterology, Veszprem, Hungary;(2)Semmelweis University, Department of Medicine and Oncology, Budapest, Hungary;(3)Hungarian Defence Forces- Medical Centre, Department of Gastroenterology, Budapest, Hungary;(4)Grof Esterhazy Hospital, Department of Gastroenterology, Papa, Hungary;(5)McGill University Health Centre, Department of Gastroenterology, Montreal, Canada;
Background
The number of epidemiological population-based studies are still limited from Eastern Europe. The present study is a continuation of the Veszprem IBD population based cohort with a follow-up of the incidence and disease course of IBD since 1977. Our aim was to analyze the incidence and disease phenotype at diagnosis, and the maximal therapeutic step distributions during follow-up in a prospective population-based database from Veszprem Province, including incident Crohn’s disease (CD) patients diagnosed between January 1, 2007 and December 31, 2018.
Methods
Data of 421 incident CD patients were analyzed (male/female: 237/184; median age at diagnosis: 29 years(y) [IQR: 21-42]). Both in-hospital and outpatient records were collected and comprehensively reviewed at diagnosis and during clinical follow-up. The source of age- and gender-specific demographic data was derived from the national population census in 2011.
Results
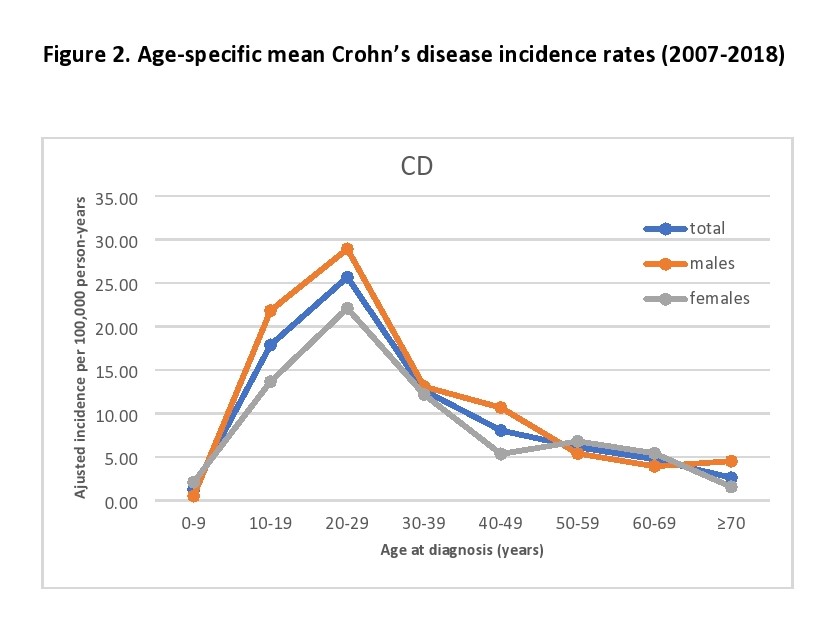
Adjusted mean incidence rate was 9.94(CI95%: 9.0-10.9)/105 person-years in this 12 year period[males:11.5(CI95%:10.2-13.2)/105; females:8.4(CI95%:7.3-9.7)/105]. Prevalence rate was 191.18(CI95%:177.0-205.7)/105 persons in 2011 and 236.78(CI95%:220.8-252.8) in 2015. For detailed annual incidence rates and age-specific mean incidence rates see Figure1 and 2. Peak onset age in CD was 20–29 years of age. Diagnostic delay from symptom onset was ≥1year in 26.6%, and ≥3 years in 10% of the patients. Disease location was ileal(L1) in 29.7%, colonic(L2) in 24.5%, and ileo-colonic(L3) in 45.8% at diagnosis. Upper gastrointestinal manifestation or perianal disease were present in 7.6% and 13.5%. Disease behavior at diagnosis was luminal(B1) in 62.5%, stenosing(B2) in 17.6%, penetrating(B3) in 16.4%, and B2+B3 in 3.6%. Patients with ileocolonic disease were younger (29.2y,SD:14.6) at diagnosis compared to patients with ileal(35.7y,SD:15.5;p<0.001) or colonic disease(37.7y;SD:18.1;p<0.001). Extraintestinal manifestations were as follows: hepatic5.0%(PSC 1.9%), arthritis13.8%, ocular1.7%, cutan4.3%. Active smokers at diagnosis were 35.4%. Distribution of maximal therapeutic steps during the course of follow-up (8.53y,SD: 3.3) were 5-ASA in 15.7%, systemic corticosteroids in 14.3%, immunosuppressive therapy in 42.5%; anti-TNF biologic therapy in 23.3% and other biologic therapy in 2.9%.

Conclusion
The incidence of CD in this 12 year period was high, comparable to high-incidence areas in Western European countries, and comparable to previous data from the Veszprem cohort, while prevalence rates continue to rise.(Lakatos 2011, IBD). Ileocolonic location and penetrating disease behavior were somewhat higher compared to previous population-based data from Western Europe.(Burisch 2018, JCC).


