D. Vranesic Bender1, V. Domislović2, M. Brinar2,3, D. Ljubas Kelečić1, I. Karas1, M. Novosel3, M. Matašin3, Ž. Krznarić1,2,3
1Unit for Clinical Nutrition, Department of Gastroenterology and Hepatology, Zagreb, Croatia, 2Clinical Hospital Centre Zagreb, Department of Gastroenterology and Hepatology, Zagreb, Croatia, 3Zagreb School of Medicine, University of Zagreb, Zagreb, Croatia
Background
Vitamin D deficiency is frequently present in inflammatory bowel disease (IBD) with a higher incidence in Crohn’s disease (CD) than in ulcerative colitis (UC). Given the involvement of the alimentary tract, many factors can contribute to vitamin D deficiency. The aim of the study was to investigate the association of vitamin D deficiency according to body mass index (BMI) in adult patients with IBD.
Methods
A cross-sectional study was conducted on a cohort of 152 IBD patients, 68.1% (n = 104) CD and 31.9% (n = 48) UC. The mean age of the total study population was 37.3±11.8 years and 57.3% (n = 87) were male. All patients were adult, Caucasian and without vitamin D supplementation. Patients were recruited during one year period.
Results
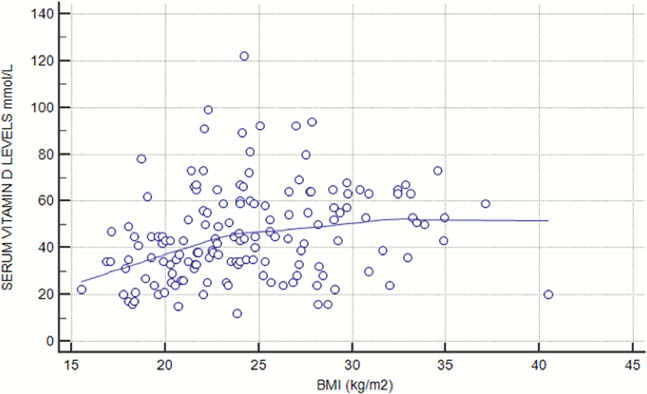
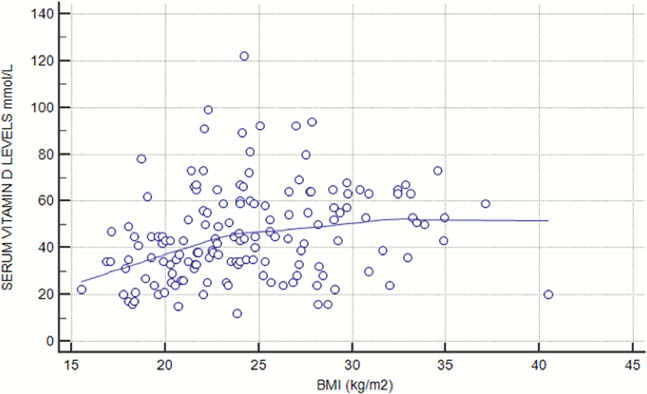
Out of all IBD patients, 60.5% (n = 92) had vitamin D deficiency, 32.2%, (n = 49) insufficiency and 7.2% (n = 11) sufficiency. According to BMI categories there were 12.5% (n = 19) obese patients, 27.6% (n = 42) overweight, 51.3% (n = 78) with normal body weight, and 8.6% (n = 13) underweight. There was a significant difference in vitamin D levels according to different BMI categories in terms of underweight patients having the lowest vitamin D levels; underweight 29.84±11.94 mmol/l, normal 46 ± 20.7 mmol/l, overweight 48±20.1 mmol/l, obese 51±15.3 mmol/l. In addition, there was a significant correlation of vitamin D levels and BMI values (Rho = 0.212, 95% CI 0.069–0.345, p = 0.004), which was more clearly observed in the lower range of BMI values (Figure 1). Male underweight patients had lower levels of vitamin D compared with female patients (26.6 ± 9 vs. 34.7 ± 5.6, p < 0.05). Both patients with CD and UC had significant positive correlation of vitamin D levels and BMI values (UC Rho=0.40, 95% CI 0.16–0.59, p = 0.001, UC Rho = 0.27, 95% CI 0.01–0.05, p = 0.044). However, when comparing vitamin D levels according to phenotype, a significant difference in vitamin D levels was observed in underweight CD (28.4 ± 11.1) comparing to underweight UC patients (40.6 ± 10.6), p < 0.05. In logistic regression analysis, CD phenotype was risk factor for vitamin D deficiency (OR 2.18 95% CI 1.01–4.72, β = 1.22, p = 0.04).
Conclusion
Our results on untreated IBD patients show a high proportion of vitamin D deficiency both in CD and UC, and significant correlation of vitamin D levels and BMI values, especially in the lower range of BMI values. Moreover, underweight CD patients have lower vitamin D levels comparing to UC. This suggests the need for regular vitamin D monitoring and supplementation especially in IBD patients at risk.