P657 Evolution of Crohn’s disease progression and surgery rates over 10 years for patients who initiated biologic treatment early compared with late or no biologic initiation
N. Pillai1, M. Dusheiko1, M. Maillard2, P. Michetti2, V. Pittet PhD1, Swiss IBD Cohort Study
1Center for Primary Care and Public Health - University of Lausanne, Epidemiology and Health Services, Lausanne, Switzerland, 2Gastroenterologie La Source-Beaulieu, Centre Crohn et Colite, Lausanne, Switzerland
Background
This study aimed to evaluate the clinical outcomes for adults diagnosed with Crohn’s disease (CD) who started biologic treatments within 2 years of diagnosis (early initiation) compared with those who started biologics >2 years after diagnosis or who did not receive any biologic treatment during the period of observation (late/no biologic initiation).
Methods
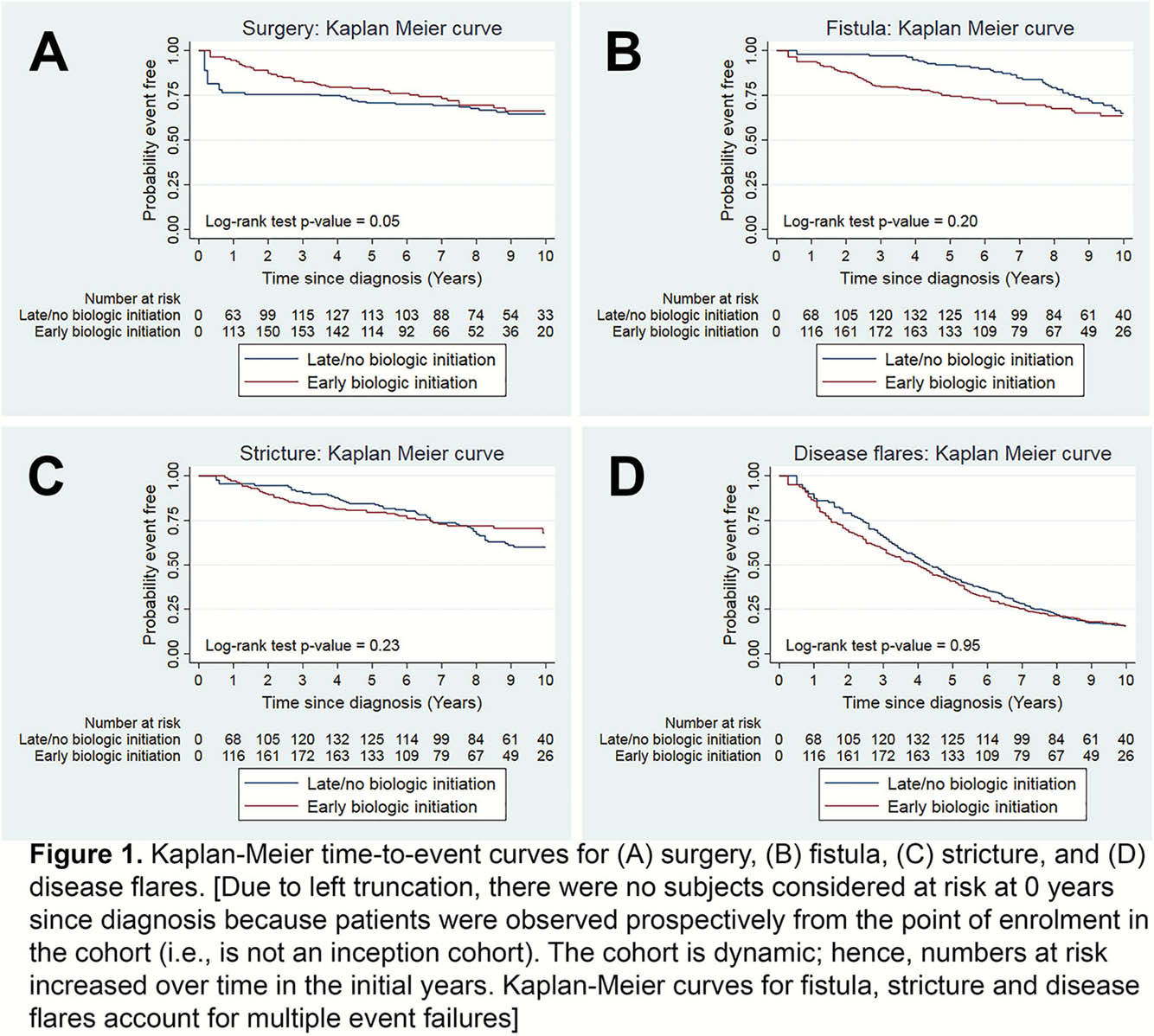
We conducted a retrospective analysis using 10 years of follow-up data from patients included in a national cohort study. We used propensity score methods to match patients in the early vs. late/no biologic initiation groups based on key baseline patient and clinical characteristics. Kaplan–Meier time-to-event models were used to evaluate the risks of intestinal resection surgery, fistula, stricture, and disease flares for each group. In addition, a subgroup analysis was performed stratifying patients known to have initiated biologic treatments into early (≤2 years after diagnosis) vs. late (>2 years after diagnosis) initiation groups.
Results
In total, 411 patients were matched in the early initiation (
Conclusion
This study found no significant differences in the long-term cumulative probabilities of intestinal resection surgery, fistula, stricture, and disease flares amongst CD patients who initiated biologic treatment early compared with similar patients who initiated biologic therapy late or who had not started any biologic treatments. However, in a subgroup of patients known to receive biologic treatments, early initiation was associated with significantly lower overall risks of strictures and disease flares. These results highlighted the need for more individualised care in CD in order to target aggressive treatment approaches to patients who show early signs of a complicated disease course.


