P659 The impact of total colectomy on the course of extraintestinal manifestations in Swiss IBD cohort study patients
R. Roth1, S. Vavrick2, M. Scharl1, P. Schreiner1, T. Greuter1, J. Zeitz3, E. Safroneeva4, A. Schoepfer5, M.P. Barry6, G. Rogler1, L. Biedermann1, Swiss IBD Cohort Study
1University Hospital Zurich, Gastroenterology and Hepatology, Zuerich, Switzerland, 2Private Practice, Center for Gastroenterology and Hepatology, Zurich, Switzerland, 3Clinic Hirslanden- Zurich- Switzerland, Center of Gastroenterology, Zurich, Switzerland, 4University of Bern, Institute of Social and Preventive Medicine, Bern, Switzerland, 5Centre Hospitalier Universitaire Vaudois CHUV and University of Lausanne, Division of Gastroenterology and Hepatology, Lausanne, Switzerland, 6Center for Primary Care and Public Health Unisanté – University of Lausanne, Institute of Social and Preventive Medicine IUMSP, Lausanne, Switzerland
Background
Extraintestinal manifestations (EIM) are reported to occur in a highly variable frequency of between 6% and up to 47% of patient with IBD during the course of disease and may substantially contribute to the overall disease burden. Little is known on the impact of colectomy in UC or CD patients on the course of EIM, neither regarding pre-existing vs.
Methods
Using data from the Swiss IBD Cohort Study (SIBDCS) we aimed to analyze the course of EIM in UC and CD patients undergoing colectomy during the prospective SIBDCS follow-up.
Results
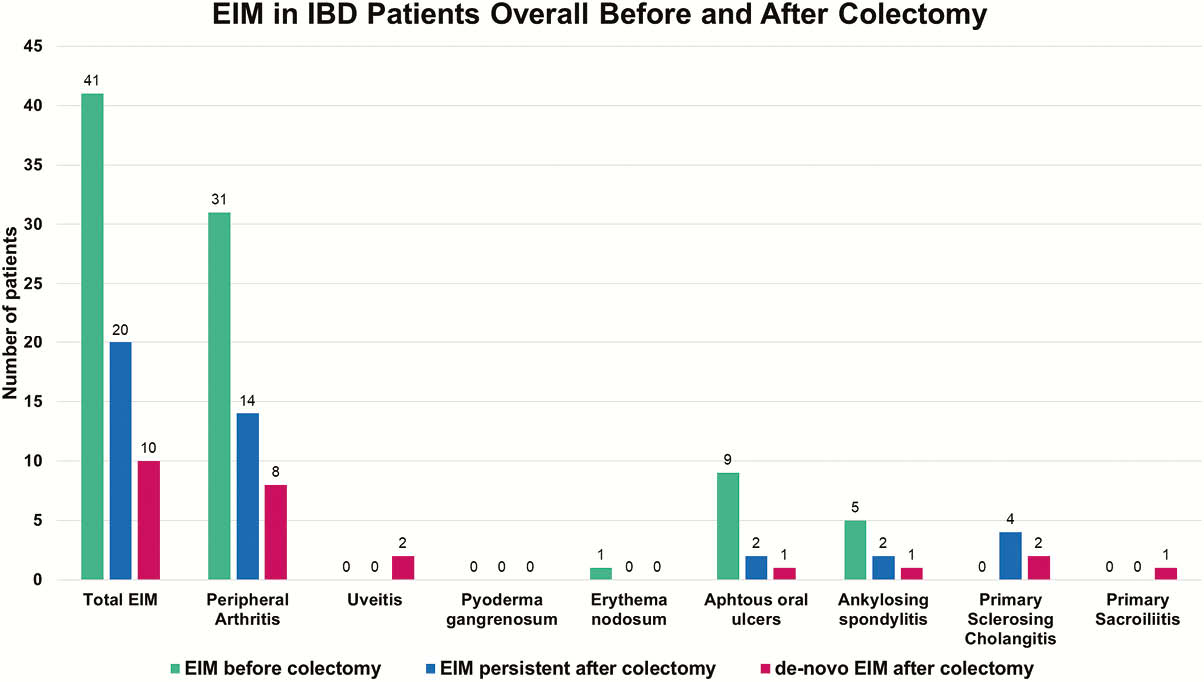
Amongst a total of 3620 IBD patients (53.6% CD, 42.8% UC, 3.6% IBD unclassified), 115 IBD patients (33 CD and 82 UC) underwent colectomy. One or more EIM had been present at any time antecedent to colectomy in 35.7% of these patients (27.3% and 39% in CD and UC patients, respectively). Within the 115 IBD patients undergoing colectomy any EIM was present only before colectomy in 21 patients (18.3% of all patients undergoing colectomy), i.e. entirely ceased thereafter in 51.2% of patients with any EIM prior to colectomy. After colectomy, overall 30 out of the 115 patients (26.1%) suffered from any EIM after colectomy. Out of these, two thirds (20 patients) already had any EIM prior to colectomy, while in one third (10 patients) occurrence of EIM represented a de-novo event after colectomy. Overall, amongst all patient with no EIM prior to undergoing colectomy 13.5% of patients developed a de-novo EIM after colectomy. The fraction of patients with complete cessation of EIM after colectomy was numerically higher in patients with UC vs. CD with 56.3% vs. 33.3% of patients with EIM prior to colectomy, respectively (51.2% in IBD patients overall). An overview over the frequency of EIM overall and individual EIM is provided in Figure 1.
Conclusion
In IBD patients with undergoing colectomy, any EIM present prior to surgical intervention will persist in about half of patients. Although our results are based on a limited number of patients our findings indicate, that complete cessation of EIM after colectomy may be less common in CD than in UC patients. Absence of EIM prior to colectomy does not equal freedom from any EIM thereafter as up to one in seven IBD patients may develop de-novo EIM after colectomy.


