P665 Cardiovascular risk profile in chronic auto-inflammatory diseases: a cross-sectional single center study
Sleutjes, J.A.M.(1);Roeters van Lennep , J.E.(2);Verploegh , P.J.P.(1);van Doorn , M.B.A.(3);Vis , M.(4);van der Woude , C.J.(1);de Vries , A.C.(1);
(1)Erasmus Medical Center, Gastroenterology & Hepatology, Rotterdam, The Netherlands;(2)Erasmus Medical Center, Internal Medicine, Rotterdam, The Netherlands;(3)Erasmus Medical Center, Dermatology, Rotterdam, The Netherlands;(4)Erasmus Medical Center, Rheumatology, Rotterdam, The Netherlands
Background
Background
Chronic auto-inflammatory diseases are associated with an increased risk of arterial and venous cardiovascular diseases (CVD). Pathogenesis may be related to chronic inflammation and/or traditional CVD risk factors. We aimed to assess the prevalence of CVD and cardiovascular risk profile in inflammatory bowel disease (IBD), psoriasis (PSO) and spondylarthropathies (SpA).
Methods
Methods
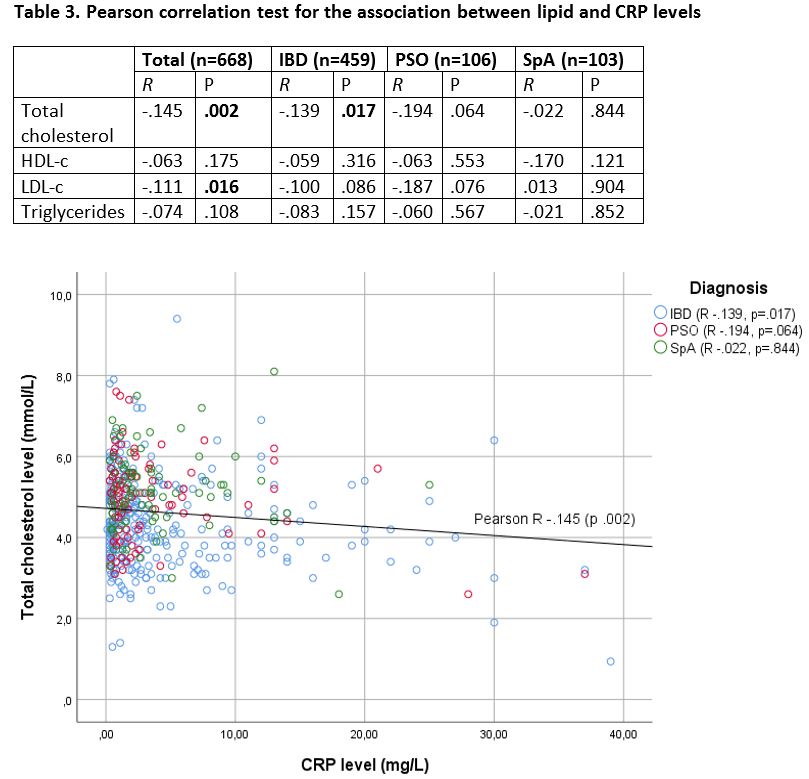
This is a single center cross-sectional study at the depts. of Gastroenterology, Dermatology and Rheumatology. Patients ≥18 years underwent body measurements (blood pressure (BP), BMI, waist and hip circumference), laboratory analysis (plasma glucose, lipid spectrum) and completed a cardiovascular questionnaire (e.g. history of CVD, medication use). Multivariate linear and logistic regression models corrected for age and sex were applied to identify differences between groups.. Sensitivity analyses were performed excluding patients taking statins or anti hypertensive drugs. Within groups, association between lipid levels and clinical disease activity was assessed by stratification, and with CRP levels by Pearson correlation test.
Results
Results
A total of 668 patients were included (335 males (50%), median age 47 years: 459 IBD (69%), 106 PSO (16%) and 103 SpA patients (15%). (Table 1) The prevalence of venous thromboembolisms was 6%, heart failure 3% and arterial CVD 8%. IBD patients had lower BMI, systolic BP, TC and LDL-c levels, and lower odds ratio of having diabetes, overweight and hypercholesterolemia, as compared to PSO and SpA, but a higher odds ratio of having VTE. (Table 2) These results were independent of statin of anti hypertensive drug use. All groups showed a trend towards higher levels of TC, HDL-c and LDL-c during disease remission as compared to active disease (Figure 1) Overall, TC and LDL-c levels were inversely correlated with CRP (R -.145, p=.002 and R -.111, p=.016); within groups a significant association was only observed in IBD. (Table 3, Figure 2)


Conclusion
Conclusion
IBD patients have a more favorable cardiovascular risk profile, as compared to PSO and SpA. Screening and early intervention for CVD risk factors requires different strategies for each population.


