P672 The escalation of therapy or intervention (ETI) calculator for ulcerative colitis: does it have the potential to help outpatient capacity meet demand?
A.J. Walsh, L. Matini, R. Kantschuster, M. Lepetyukh, D. Simadibrata, G. Collins, J. Wilson, M. Hussain, A. Tarafdar, O. Brain, R. Palmer, T. Ambrose, J. Satsangi, S.P.L. Travis
Oxford University Hospitals NHS Foundation Trust and Oxford AHSN, Translational Gastroenterology Unit, Oxford, UK
Background
Demand for outpatient clinic appointments for ulcerative colitis (UC) often exceeds capacity, since spaces are frequently assigned to routine follow-up of patients who are well. Demand might better be managed by targeting appointments for patients in need of therapeutic decisions. The TrueColours UC (TCUC) Escalation of Therapy or Intervention (ETI) calculator is a potential enabling tool.
Methods
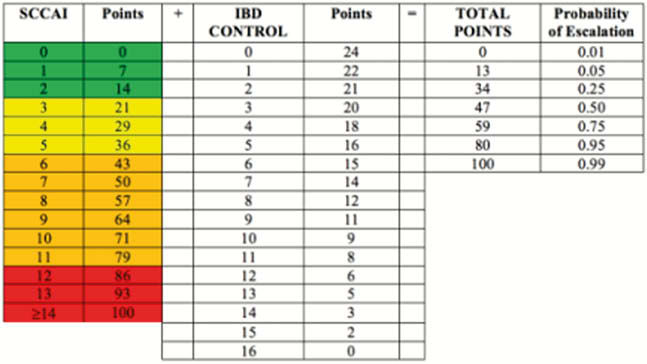
TCUC is a web-based programme based on email prompts linked to validated, disease-specific indices. The ETI Calculator was created after logistic regression showed that patient-reported symptoms (Simple Clinical Colitis Activity Index) and quality of life (IBD Control-8) could calculate the probability of therapy escalation or an urgent intervention during an outpatient appointment (OPA, Figure 1). From June 2018 to August 2019, all OPA for 650 patients using TCUC and under standard OPA follow-up were examined. The probability of escalation at each OPA was calculated using the most recent prior SCCAI and IBD-Control scores (within 2 weeks of appointment). Clinic letters were assessed to determine whether treatment escalation or intervention had occurred during the OPA.
Results
Of 650 patients, 236 had a total of 403 OPAs. 210/403 (52%) of these OPAs resulted in no treatment escalation; 159/403 (40%) had escalation and 34/410 (8%) had de-escalation. An ETI calculator threshold set at 5% estimated probability of treatment escalation would have correctly identified 143/159 (90%) escalation events. 16/159 (10%) escalations were not correctly predicted: 12/16 were escalations of medication (oral 5-aminosalicylic acid,
Conclusion
A model that predicts the likelihood of treatment escalation or intervention during an OPA, based on real-time data entered by patients, has the potential to improve outpatient clinic resource utilisation. The calculator may not be valid to triage patients recently on steroids.


