P689 Patient-reported outcomes (PRO-2) and intestinal ultrasound in ulcerative colitis patients: subanalysis of the TRUST&UC study cohort
C. Maaser1, U. Helwig2, I. Fischer3, S. Rath4, S. Kolterer4, T. Kucharzik5
1Hospital Lüneburg, Outpatients Department of Gastroenterology, Lüneburg, Germany, 2Gastroenterology Practice, n.a., Oldenburg, Germany, 3Biostatistik Tuebingen, n.a., Tuebingen, Germany, 4AbbVie Deutschland GmbH & Co. KG, Medical Department, Wiesbaden, Germany, 5University Teaching Hospital Lueneburg, Department of Internal Medicine and Gastroenterology, Lueneburg, Germany
Background
Patient-reported Outcomes (PRO) are gaining increasing acceptance as new tools to evaluate clinical activity, especially in the context of clinical trials and evaluation of drug efficacy. However, data to support the relevance of these endpoints and their correlation to objective markers of inflammation is still lacking.1 Recently published data demonstrated the feasibility of intestinal ultrasound (IUS) as a routine monitoring technique in clinical practice for Crohn’s disease (CD) and ulcerative colitis (UC) patients.2 Thus, the importance and significance of IUS, as a patient-centric and non-invasive technique has emerged over the last years and will become more relevant in the future.With this sub-analysis of the TRUST&UC study, we aimed to investigate the correlation between improvement in ultrasound parameters and PRO-2 in UC patients.
Methods
TRUST&UC is a prospective, observational study including 244 patients with an increased bowel wall thickness (BWT) at baseline and active UC (SCCAI ≥ 5). These patients were analysed for the Simple Clinical Colitis Activity Index (SCCAI) subscores stool frequency, urgency and rectal bleeding. These parameters were documented for up to 4 visits (baseline, an optional visit at week 2, week 6 and week 12). Pathological stool frequency was defined as a stool frequency of ≥1 point (≥ 4 stools/day) and pathological rectal bleeding was defined as ≥1 point (traces of blood in stool); the combination of both subscores was defined as PRO-2.
Results
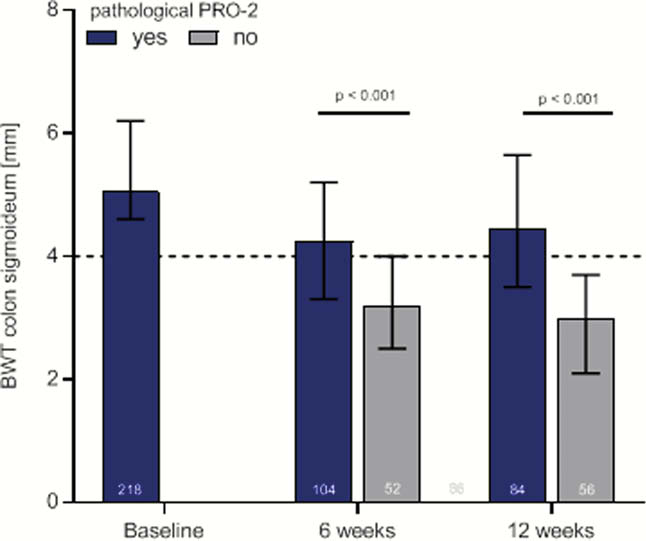
We found a positive moderate correlation between BWT and the investigated SCCAI-subscores (rectal bleeding and BWT at W12
Conclusion
With this sub-analysis of the TRUST&UC study we demonstrated that bowel wall thickness, assessed by intestinal ultrasound, had a moderate correlation with normalisation of patient-reported outcomes as early as week 6 and 12. Furthermore, patients with non-pathological PRO-2 had significantly decreased bowel wall thickness. This again supports the value of intestinal ultrasound in routine medical practice.
Sandborn WJ,
Kucharzik T,
Restellini S,


