P695 Attitudes and predictors of COVID-19 vaccine uptake in patients with Inflammatory Bowel Disease
Zhang, E.(1);Gupta, A.(1);Macrae, F.A.(1);Christensen, B.(1);
(1)Royal Melbourne Hospital, Gastroenterology, Melbourne, Australia;
Background
Vaccination has proven to be an effective public health measure to combat the SARS-CoV-2 pandemic. However, vaccine “hesitancy” has limited uptake in some populations. We surveyed individuals with IBD to explore factors associated with vaccine uptake, concerns, and which sources of information were considered trustworthy surrounding vaccination.
Methods
Patients with IBD were recruited from a specialist IBD clinic at a tertiary hospital in Australia, and through a national IBD patient society (Crohn’s & Colitis Australia). Patients were invited to complete an anonymous survey between 31 October – 17 November 2021. Logistic regression was used to identify variables associated with vaccine uptake. Data was analysed using SPSS (Chicago, IL).
Results
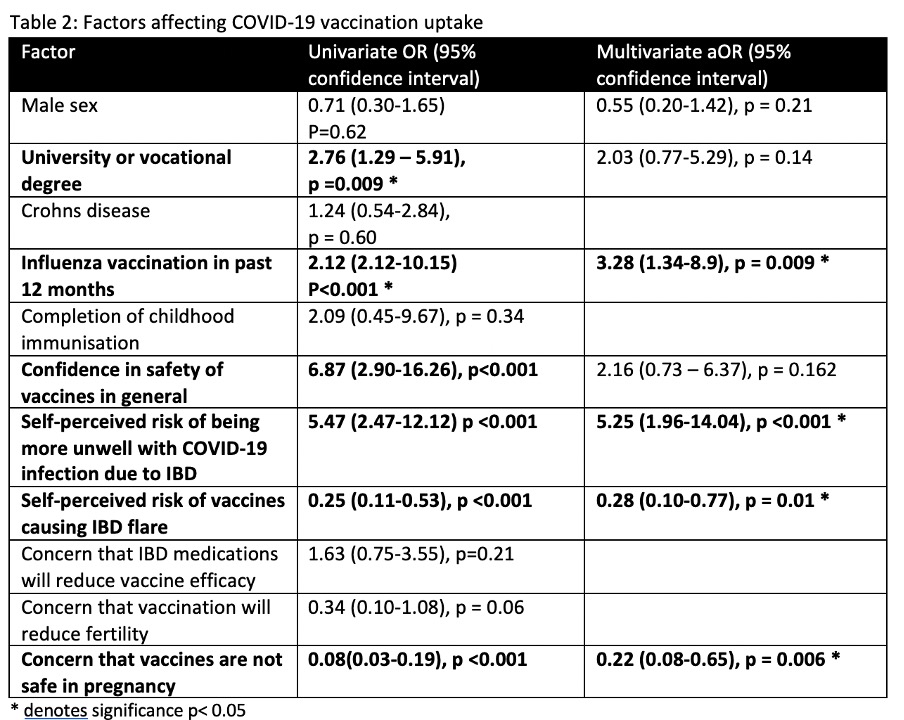
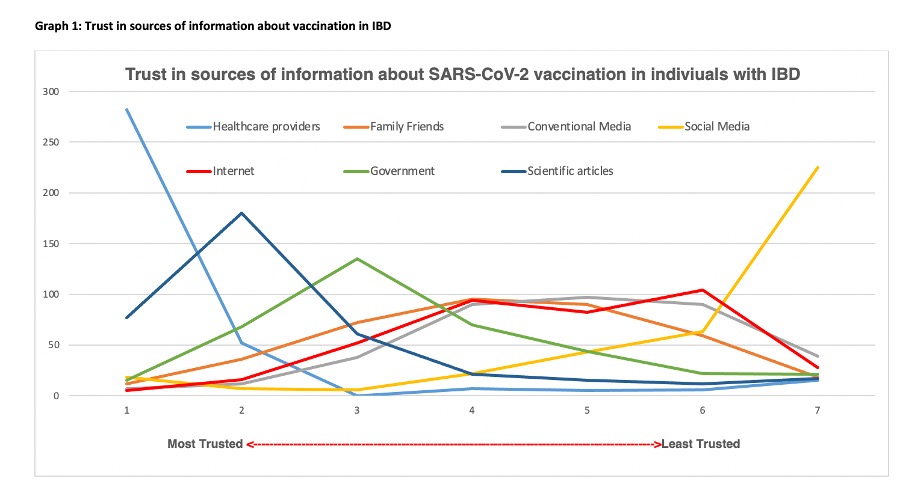
There were a total of 441 respondents. Demographic and IBD characteristics are presented in Table 1. Most respondents 411 (93.2%) had received at least 1 dose of COVID-19 vaccination. Among 30 (6.8%) respondents who had not been vaccinated, concern about experiencing an IBD flare with vaccination and vaccine safety were most commonly identified. Of those who had not yet been vaccinated, the possibility of getting vaccinated in the future was likely in 3 (10.7%), unlikely in 12 (42.8%), whilst 13 (45.4%) were unsure about future vaccination. Multivariate analysis [Table 2] demonstrated past influenza vaccination (OR 3.28, 95% CI 1.34-8.9, p = 0.009) and self-perceived risk of being more unwell with COVID-19 infection due to IBD was positively associated with COVID-19 vaccine uptake (OR 5.25, 95% CI 1.96-14.04, p <0.001). Most agreed that that vaccination in general was safe 306 (90.1%). The perceived risk of COVID-19 vaccination causing an IBD flare, and concern that vaccination is unsafe in pregnancy were both negatively associated with vaccine uptake (OR 0.28, 95% CI 0.10-0.77, p = 0.01 and OR 0.22, 95% CI 0.08-0.65, p = 0.006) respectively. Trust in healthcare workers was high with 282 (73.7%) responders ranking them the most trusted source to obtain information surrounding vaccination [Figure 1]. Social media was ranked the least trusted source of information by 225 (58.6%).
Conclusion
Past influenza vaccination and self-perceived risk of being more unwell with COVID-19 due to IBD, were positive predictors of COVID-19 vaccine uptake in IBD patients. Concerns about an IBD flare with vaccination is a unique consideration in those vaccine hesitant and is a negative predictor of vaccine uptake. Among those not yet vaccinated, 45% were uncertain about future vaccination. Given healthcare providers were ranked the most trusted source surrounding this domain, this survey highlights the key role they have in exploring vaccination concerns and misconceptions in IBD patients


