P744 Epidemiology, clinical characteristics, evolution and treatments in newly diagnosed inflammatory bowel disease (IBD): Results from the nationwide EpidemIBD study of GETECCU
M. Chaparro1, M. Barreiro-de Acosta2, J.M. Benítez3, J.L. Cabriada4, M.J. Casanova1, D. Ceballos5, M. Esteve6, H. Fernández7, D. Ginard8, F. Gomollón9, R. Lorente10, P. Nos11, S. Riestra12, M. Rivero13, P. Robledo14, C. Rodríguez15, B. Sicilia16, E. Torrella17, A. Garre1, F. Rodríguez-Artalejo18, E. García-Esquinas18, J.P. Gisbert1, on behalf of the EpidemIBD group of GETECCU
1Hospital Universitario de La Princesa- IIS-IP- Universidad Autónoma de Madrid and CIBEREHD, Gastroenterology Unit, Madrid, Spain, 2Complexo Hospitalario Universitario de Santiago, Gastroenterology Unit, Santiago de Compostela, Spain, 3Hospital Universitario Reina Sofía and IMIBIC, Gastroenterology Unit, Córdoba, Spain, 4Hospital de Galdakao-Usansolo, Gastroenterology Unit, Vizcaya, Spain, 5Hospital Universitario de Gran Canaria Dr. Negrin, Gastroenterology Unit, Las Palmas, Spain, 6Hospital Universitari Mutua Terrasa and CIBERehd, Gastroenterology Unit, Tarrasa, Spain, 7Hospital San Pedro, Gastroenterology Unit, Logroño, Spain, 8Hospital Universitari Son Espases, Gastroenterology Unit, Palma de Mallorca, Spain, 9Hospital Clínico Universitario ‘Lozano Blesa’- IIS Aragón and CIBEREHD, Gastroenterology Unit, Zaragoza, Spain, 10Hospital General Universitario de Ciudad Real, Gastroenterology Unit, Ciudad Real, Spain, 11Hospital Universitari i Politecnic La Fe and CIBEREHD, Gastroenterology Unit, Valencia, Spain, 12Hospital Universitario Central de Asturias and ISPA, Gastroenterology Unit, Oviedo, Spain, 13Hospital Universitario Marqués de Valdecilla, Gastroenterology Unit, Santander, Spain, 14Hospital Universitario San Pedro de Alcántara, Gastroenterology Unit, Cáceres, Spain, 15Complejo Hospitalario De Navarra, Gastroenterology Unit, Pamplona, Spain, 16Hospital Universitario de Burgos, Gastroenterology Unit, Burgos, Spain, 17Hospital General Universitario J.M. Morales Meseguer, Gastroenterology Unit, Murcia, Spain, 18Universidad Autónoma de Madrid/IdiPaz and CIBERESP, Preventive Medicine and Public Health, Madrid, Spain
Background
Very few studies have reported updated data on the incidence, clinical evolution and treatment of inflammatory bowel disease (IBD) in Europe.
Methods
i) To assess the incidence of IBD in Spain; ii) to describe the main epidemiological and clinical characteristics of patients at diagnosis and the evolution of the disease; and iii) to explore the use of drug treatments in the biological era.
Results
Prospective and population-based nationwide registry. Adult patients diagnosed with IBD -Crohn’s disease (CD), ulcerative colitis (UC) or IBD unclassified (IBD-U)- during 2017 in all the 17 Spanish administrative regions were included and will be followed-up for 5 years after diagnosis. Treatment was grouped into 5 categories: mesalazine (oral or topical), steroids (intravenous, oral or topical), immunomodulators (thiopurines, methotrexate or cyclosporine), biologics (anti-TNF, vedolizumab or ustekinumab) and surgery.
Conclusion
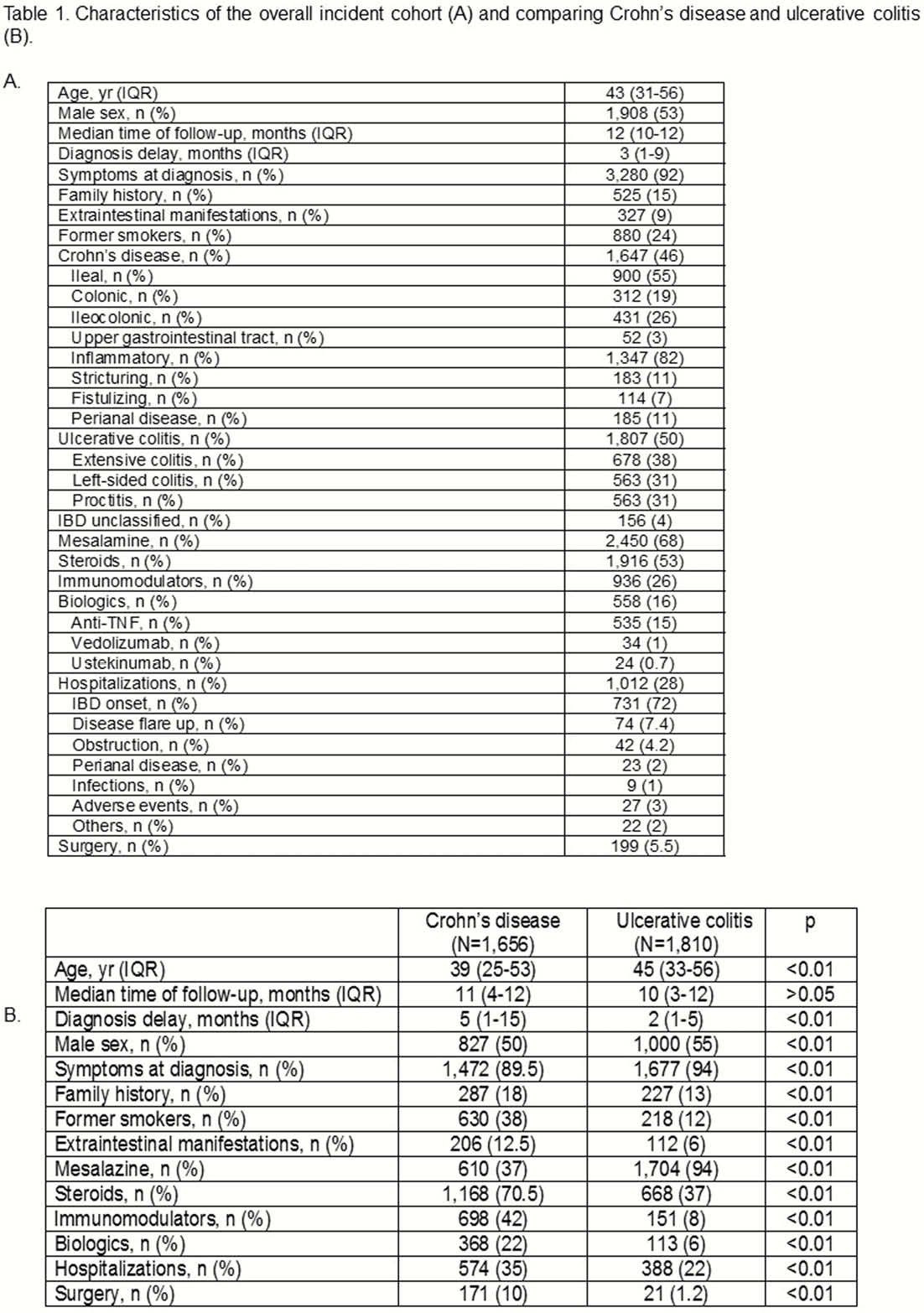
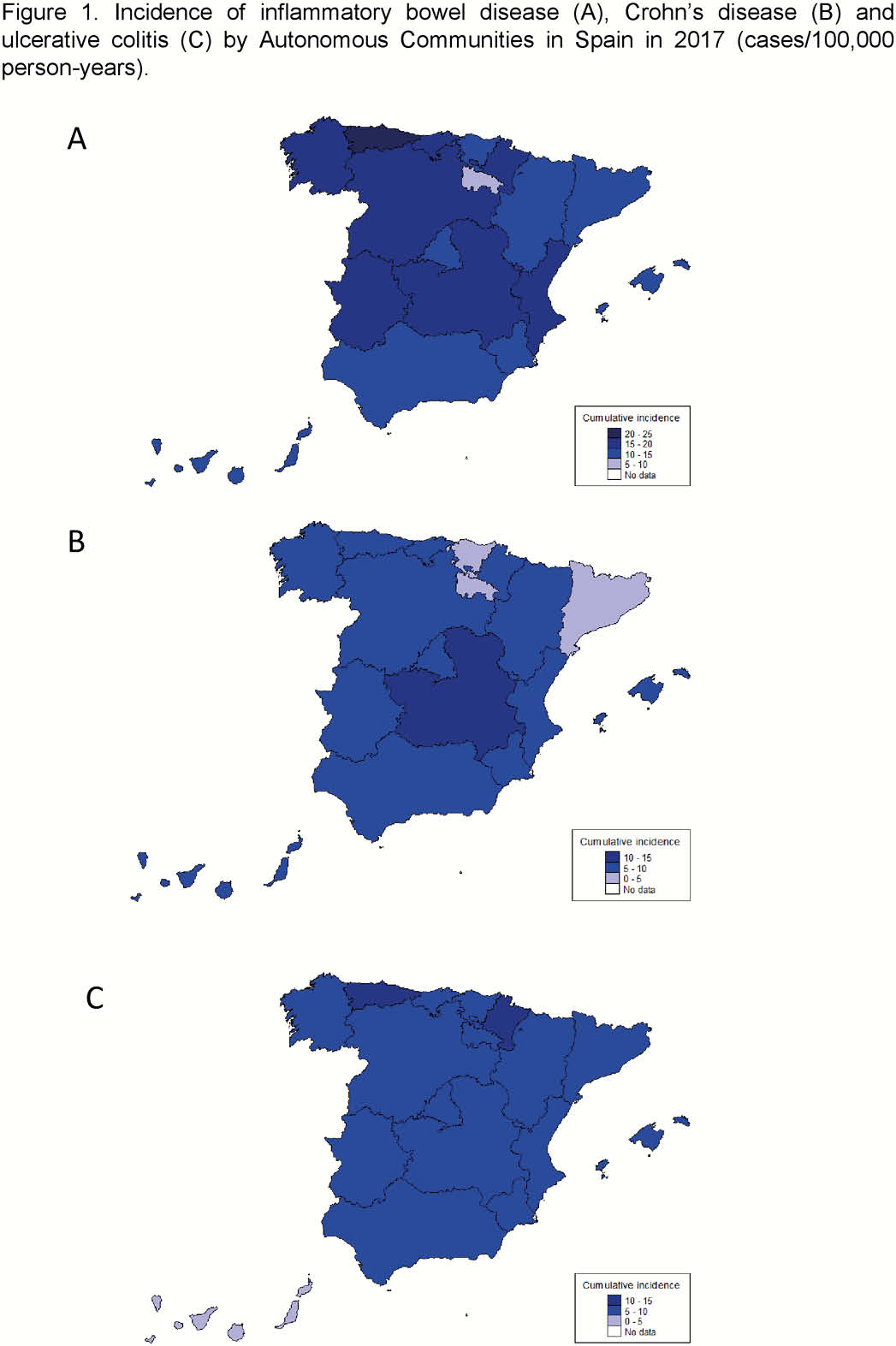
3627 incident cases of IBD diagnosed during 2017 in 108 hospitals covering over 22 millions of adult inhabitants (about 50% of the Spanish population) comprise the study cohort (Table 1). The overall incidence (cases/100.000 person-years) was 16 for IBD, 7.5 for CD, 8 for UC, and 0.5 for IBD-U. Incidence of CD was somewhat higher in Central Spain, while that of UC was higher in Northern Spain (Asturias and Navarra) (Figure 1). About 46% of patients had CD and 50% UC. Diagnosis delay was longer in CD than in UC (5 vs. 2 months,
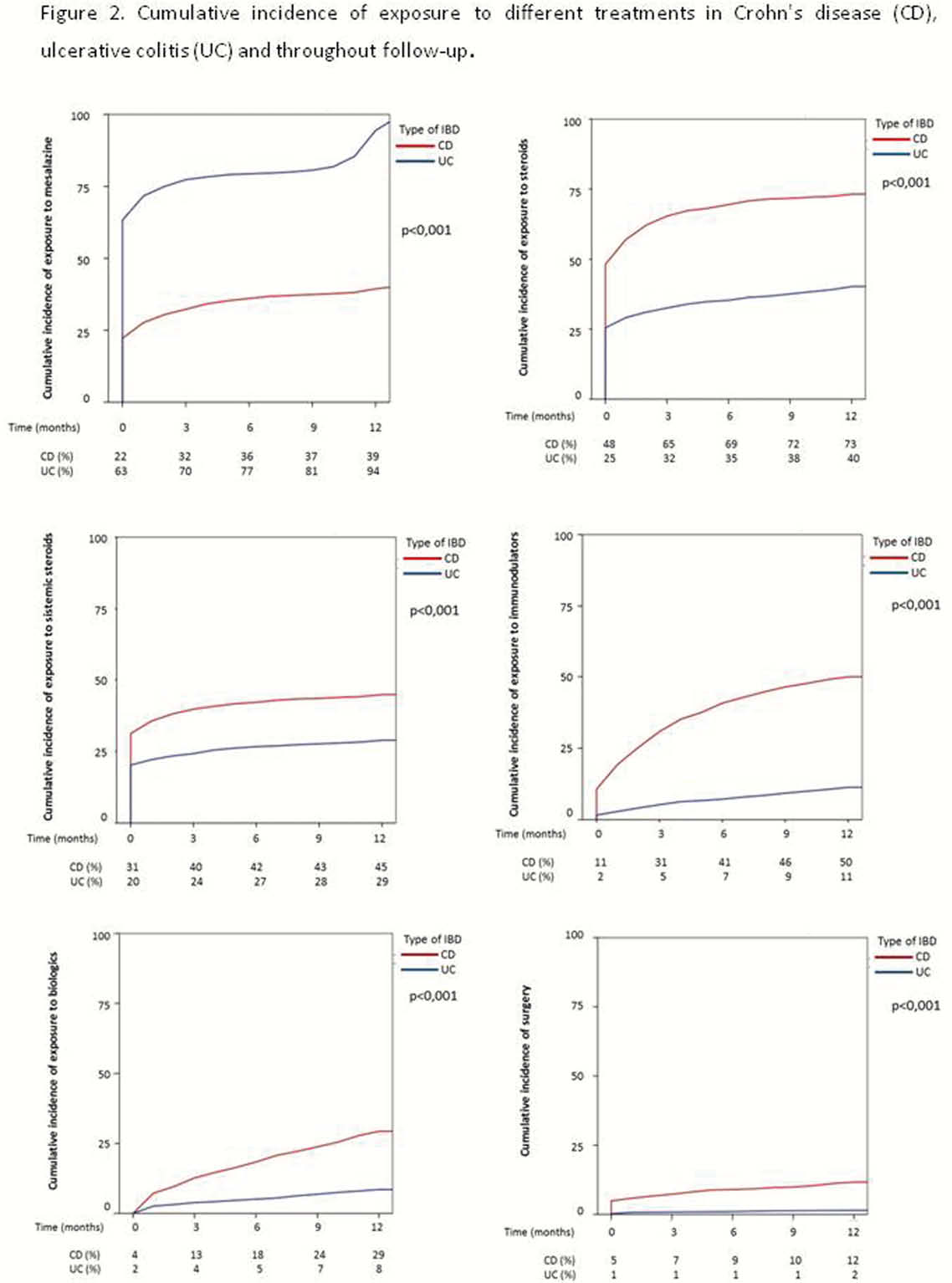
The incidence of IBD in Spain is quite high and similar to that reported in Northern Europe. IBD patients require the use of substantial therapeutic resources, which are greater in CD than in UC, and much greater than previously reported. One third of patients are hospitalised in the first year after diagnosis and over 5% undergo surgery. These results highlight the high burden of IBD as well as some of the important challenges faced by clinicians and healthcare systems to manage this costly and complex disease.


