P751 Prevalence and risk factors of non-alcoholic fatty liver disease in inflammatory bowel diseases
P. Hoffmann1, V. Jung1, R. Behnisch2, A. Gauss1
1Universitätsklinikum Heidelberg, Department of Gastroenterology and Hepatology, Heidelberg, Germany, 2Universitätsklinikum Heidelberg, Department of Medical Biometry, Heidelberg, Germany
Background
Non-alcohol fatty liver disease (NAFLD) is a widespread disease in Europe with a prevalence of 20–30% in the German population. Some studies have revealed even higher prevalence in patients with inflammatory bowel diseases (IBD). The majority of prior studies on this subject are cross-sectional analyses. Longitudinal data for the identification of prognostic parameters are missing.
Methods
This is a monocentric retrospective study encompassing both a cross-sectional and a longitudinal part. The study included 440 patients with Crohn’s disease (CD) and 254 patients with ulcerative colitis (UC). Inclusion criteria were diagnosis of IBD, age >17 years, and having received at least one abdominal ultrasound of the liver at the IBD outpatient clinic of the Heidelberg University Hospital. Exclusion criteria were presence of any infectious liver disease, alcoholic fatty liver disease, or documented abuse of alcohol. NAFLD was defined by echogenicity via ultrasoud and assigned in degrees of severity (no, mild, moderate or severe steatosis). As potential risk factors for the development of NAFLD, demographic characteristics, IBD activity (clinical scores, laboratory results, endoscopic or ultrasound findings), and IBD medications were investigated.
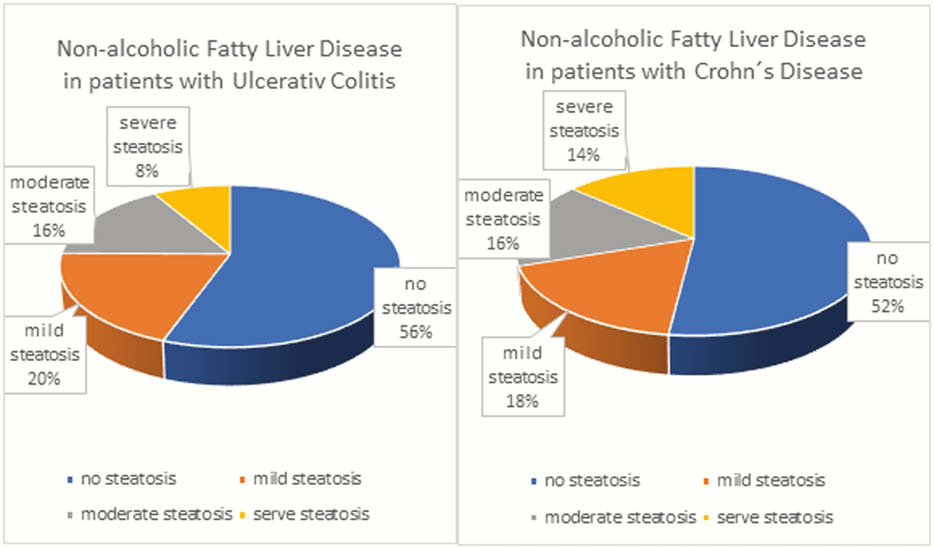
Results
The prevalence of NAFLD was 48% in CD patients and 44% in UC patients. Higher age and body mass index (BMI) were significantly associated with the occurrence of NAFLD. NAFLD was associated with higher Harvey Bradshaw Index in CD patients, while laboratory results, endoscopic or ultrasound findings proving inflammation were not associated with NAFLD. In UC patients, there was no association between disease activity and NAFLD.
The use of steroids, immunomodulators or biologics was not associated with NAFLD, while the use of sulfasalazine was associated with NAFLD only in CD patients.
In the longitudinal part of this study, 2467 hepatic ultrasound results were included. Age and BMI in CD patients and BMI in UC patients were significant risk factors in the mixed logistic regression model. Also, in CD patients, higher HBI, former bowel resections, endoscopic disease activity and use of azathioprine–not of steroids–were risk factors of NAFLD. In UC patients, endoscopic disease activity was significantly associated with NAFLD in the mixed logistic regression model.
Conclusion
There is a high prevalence of NAFLD in German IBD patients. The risk to develop NAFLD increases in older patients and patients with higher BMI. Disease activity and azathioprine use in CD may increase the prevalence of NAFLD. Our study provides a rationale for regular ultrasound screening of the liver in IBD patients.


