P810 Geriatric impairments in older inflammatory bowel disease patients are associated with higher disease burden: results of a multicentre cohort study
V. Asscher1, S. Waars1, A. van der Meulen-de Jong1, R. Stuyt2, S. Brouwer2, S. van der Marel3, J. Haans4, F. van Deudekom5, S. Mooijaart5,6, J. Maljaars1
1Leiden University Medical Center, Department of Gastroenterology and Hepatology, Leiden, The Netherlands, 2Haga Teaching Hospital, Department of Gastroenterology and Hepatology, Den Haag, The Netherlands, 3Haaglanden Medical Centre, Department of Gastroenterology and Hepatology, Den Haag, The Netherlands, 4Maastricht University Medical Center, Department of Gastroenterology and Hepatology, Maastricht, The Netherlands, 5Leiden University Medical Center, Department of Gerontology and Geriatrics, Leiden, The Netherlands, 6Institute for Evidence-Based Medicine in Old Age IEMO, Institute for Evidence-Based Medicine in Old Age IEMO, Leiden, The Netherlands
Background
The population of older patients with Inflammatory Bowel Diseases (IBD) is expanding. Knowledge on the prevalence and impact of geriatric impairments is scarce in this heterogenous group. In other fields of medicine, it has been established that geriatric impairments associate with adverse outcomes. Therefore, the aims of our study were to assess the prevalence of geriatric impairments in older IBD patients and to evaluate the association between geriatric impairments and disease burden of IBD through the short Inflammatory Bowel Disease Questionnaire (sIBDQ).
Methods
Consecutive IBD patients aged ≥65 years were included at outpatient departments and infusion centres of four hospitals in The Netherlands. Comorbidity, polypharmacy and malnutrition (somatic domain), cognitive impairment and depressive symptoms (mental domain), handgrip strength and gait speed (physical domain) and impairments in (instrumental) activities of daily living ((I)ADL) (functional domain) were assessed. Disease activity was assessed through Harvey Bradshaw Index (HBI) or partial Mayo Score (pMS) (remission: HBI<5 or pMS<2); The sIBDQ was used to assess IBD disease burden. Association between geriatric impairments and sIBDQ was assessed using multiple linear regression, including confounders age, sex, IBD type, disease duration and disease activity.
Results
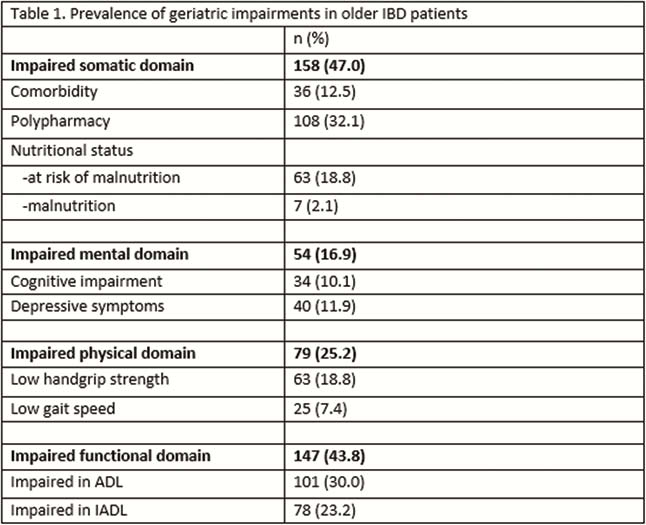
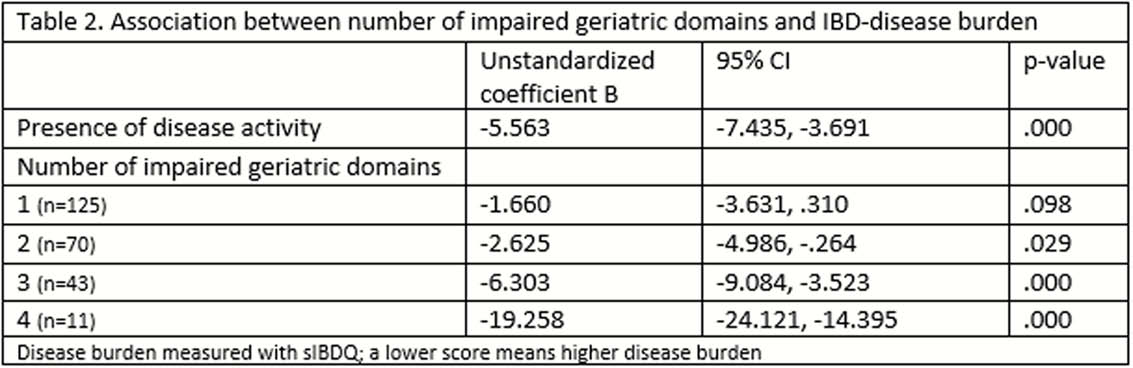
In total, 336 patients were included: median age 70.0 (IQR 67.0–73.0); 161 CD (47.9%); 71 active disease (21.1%); mean sIBDQ 59.7 (SD 8.1). Prevalence of geriatric impairments is tabulated (Table 1). Both active disease and the presence of two or more impaired domains were statistically significantly and independently associated with a higher disease burden (lower sIBDQ) (Table 2).
Conclusion
In an older IBD patient population, geriatric impairments are frequently encountered and associate with a higher disease burden. These results are a call for more research on the relationship between geriatric impairments and IBD disease burden to improve patient care in older IBD patients.


