P813 Inflammatory bowel disease in older patients: experience at a single centre
M.M. Diaz Alcazar, P. Martinez Tirado, B. Vidal Vilchez, B. Zuñiga de Mora Figueroa
Hospital Universitario San Cecilio, UGC Aparato Digestivo, Granada, Spain
Background
The characteristics of inflammatory Bowel Disease (IBD) seem different according to the age of the patient at diagnosis. Moreover, age influences the evolution of the disease. The aim of the study was to know the prevalence of IBD in patients older than 65 years old and the evolution of the disease at this age.
Methods
Retrospective descriptive study. Database from patients of the Hospital Universitario San Cecilio of Granada (Spain). 50 patients with 65 years old or more and 50 under this age have been randomly selected. Their electronic clinical records have been reviewed.
Results
The IBD Unit in our Hospital serves 1218 people with this disease, of whom 212 are elderly patients (17.4%). In the serie of 100 randomly selected patients, mean age is 58.42 years. The disease began before 65 years old in 74% of elderly patients.
| 35 (70%) | 21 (42%) | |
| 14 (28%) | 29 (58%) | |
| - Inflammatory CD | 64% | 62% |
| - Penetrating CD | 7% | 24% |
| - Stricturing CD | 29% | 14% |
| 1 (2%) | 0 |
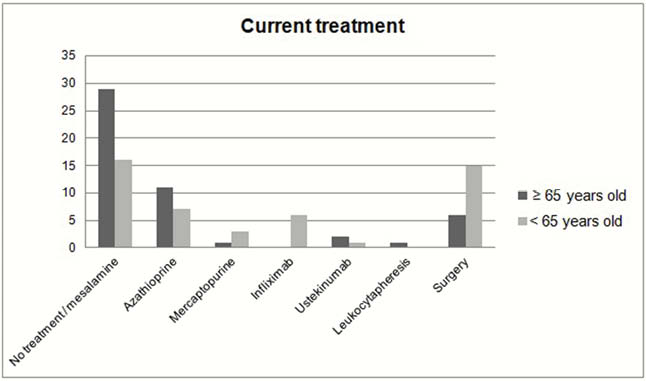
All the elderly patients continue follow-up, while 4 (8%) of the younger patients dropped out the follow-up in the IBD Unit. With regard to hospital admissions, 27 elderly patients (54%) have never required hospitalisation compared with 18 (36%) aged under 65 years. Corticosteroids were used at diagnosis in 27 (54%) of older vs. 28 (56%) of the younger patients. Meanwhile, topical treatment is used by 33 (66%) of older vs. 22 (44%) of the younger ones. The current treatment is summarised in Figure 1.
Conclusion
(1) The prevalence of IBD is increasing. IBD in older patients is also escalating due to the low mortality of the disease and the increase of patients with late-onset. In our serie, the prevalence in elderly patients is 17.4%. (2) UC is more frequent in older patients than in younger ones (70% vs. 42%). With regard to CD, penetrating disease is less frequent in older patients but stricturing pattern is more prevalent. (3) Adherence to follow-up in elderly patients is higher and they need fewer hospital admissions than younger patients. (4) In our serie, surgical and biological treatments are less frequent in elderly patients. Moreover, there are more patients above 65 years that do not take maintenance treatment or they only take mesalamine. (5) Chronological age is different from biological age. Older patients with a good quality of life should not be excluded from new treatments or clinical trials due to age. More evidence about older patients is needed to improve de diagnosis, the knowledge about the evolution and define better the treatment in this group of age.


