P829 The Burden of Colorectal Cancer in Patients with Ulcerative Colitis – Incidence and Risk factors from a Population-based Inception Cohort from Veszprem county, Western Hungary, from 1977–2020
Wetwittayakhlang, P.(1)*;Golovics , P.(2);Gonczi , L.(3);Khoury , A.(4);Kurti , Z.(5);Pandur , T.(6);David , G.(7);Erdelyi , Z.(7);Szita , I.(7);Lakatos, L.(7);LakatosPhD, P.L.(8);
(1)McGill University Health Centre, IBD Center- Division of Gastroenterology and Hepatology, Montreal- Quebec, Canada;(2)Hungarian Defence Forces Medical Centre, Department of Gastroenterology, Budapest, Hungary;(3)Semmelweis University- Budapest- Hungary, Department of Internal Medicine and Oncology, Budapest, Hungary;(4)University of Florida- Jacksonville, Division of Gastroenterology, Florida, United States;(5)Semmelweis University, Department of Internal Medicine and Oncology, Budapest, Hungary;(6)Grof Eszterhazy Hospital, Department of Gastroenterology, Papa, Hungary;(7)Ferenc Csolnoky Hospital, Department of Gastroenterology, Veszprem, Hungary;(8)Mcgill University Health Center, IBD Centre- Division of Gastroenterology and Hepatology, Montréal, Canada;
Background
Limited data are available on the incidence and risk of colorectal cancer (CRC) in ulcerative colitis (UC) from population-based studies in Eastern Europe. We aimed to identify the long-term incidence trends and predictors of CRC in a prospective population-based inception cohort from Veszprem, Western Hungary.
Methods
Patient inclusion for the inception cohort was between January 1,1977 and December 31,2018, and follow-up ended December 31,2020. The risk of CRC was estimated using standardized incidence ratios (SIRs). Age-and gender-specific CRC rates of the background population were derived from the National Cancer Registry.
Results
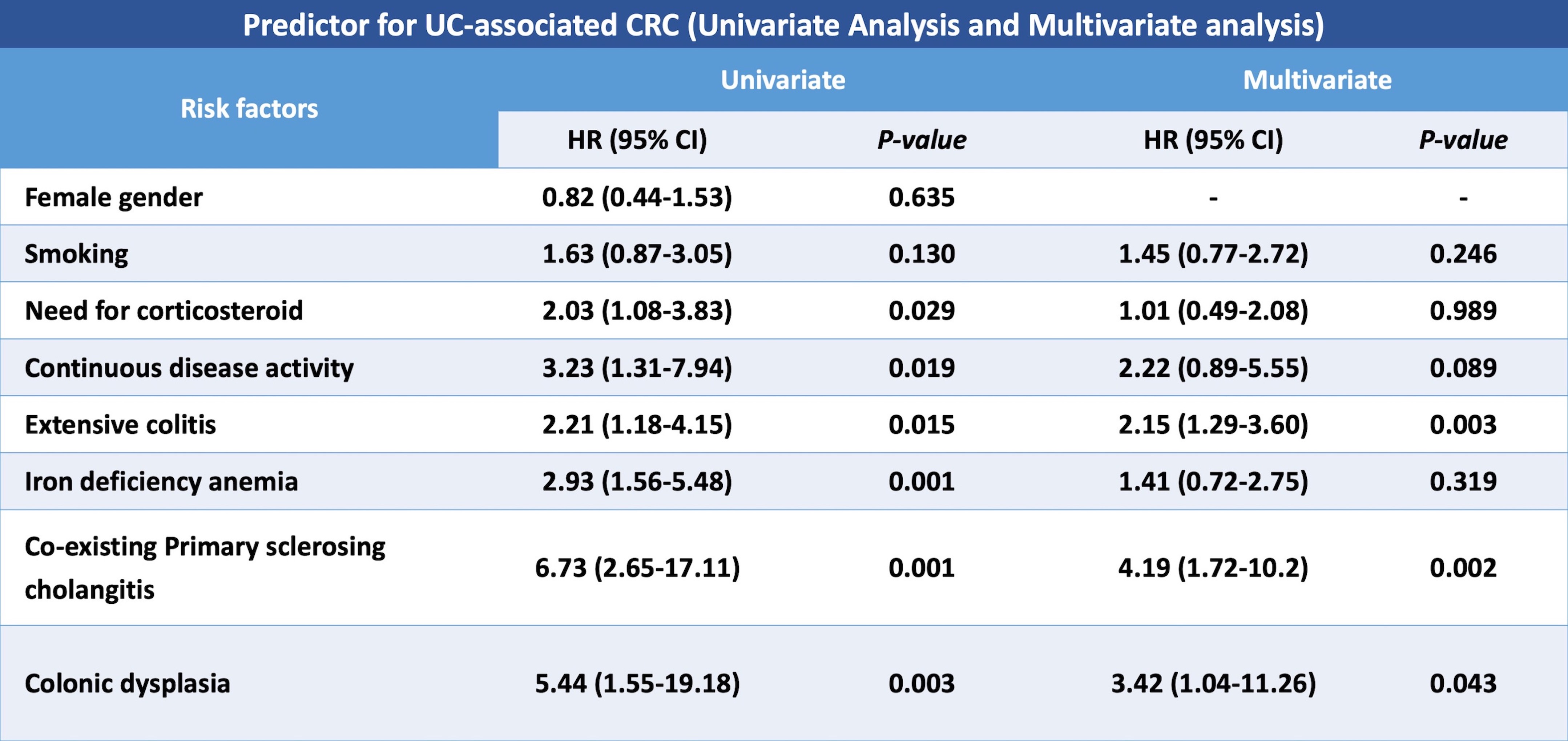
A total of 1,370 incident UC patients were included [male:51.2%, median age at diagnosis:37years). During a median follow-up of 17 years(IQR9-24), CRC was diagnosed in 41 UC patients(2.99%), equaling 1.76/1000 person-year(py).Median age at CRC diagnosis was 59(IQR:50.0-67.5) years. Overall SIR of CRC was 2.02(CI95%:10.1-12.1). SIRs were higher in extensive colitis (SIR:3.77, CI95%:2.41-5.91). The cumulative probability of CRC at 10-,20 and 30 years was 0.9% (95%CI0.6-1.2), 3.5%(95%CI2.8-4.2), and 6.5%(95%CI5.4-7.6), and there was no difference in the risk of CRC over different decades of UC diagnosis in a Kaplan Meier analysis(Log-rank=0.693). In multivariate analyses, co-existing PSC(HR4.19;95%CI1.72-10.20), colonic dysplasia(3.42;95%CI1.04-11.26), and extensive colitis (HR2.15;95%CI1.29-3.60) were identified as a significant predictor for CRC.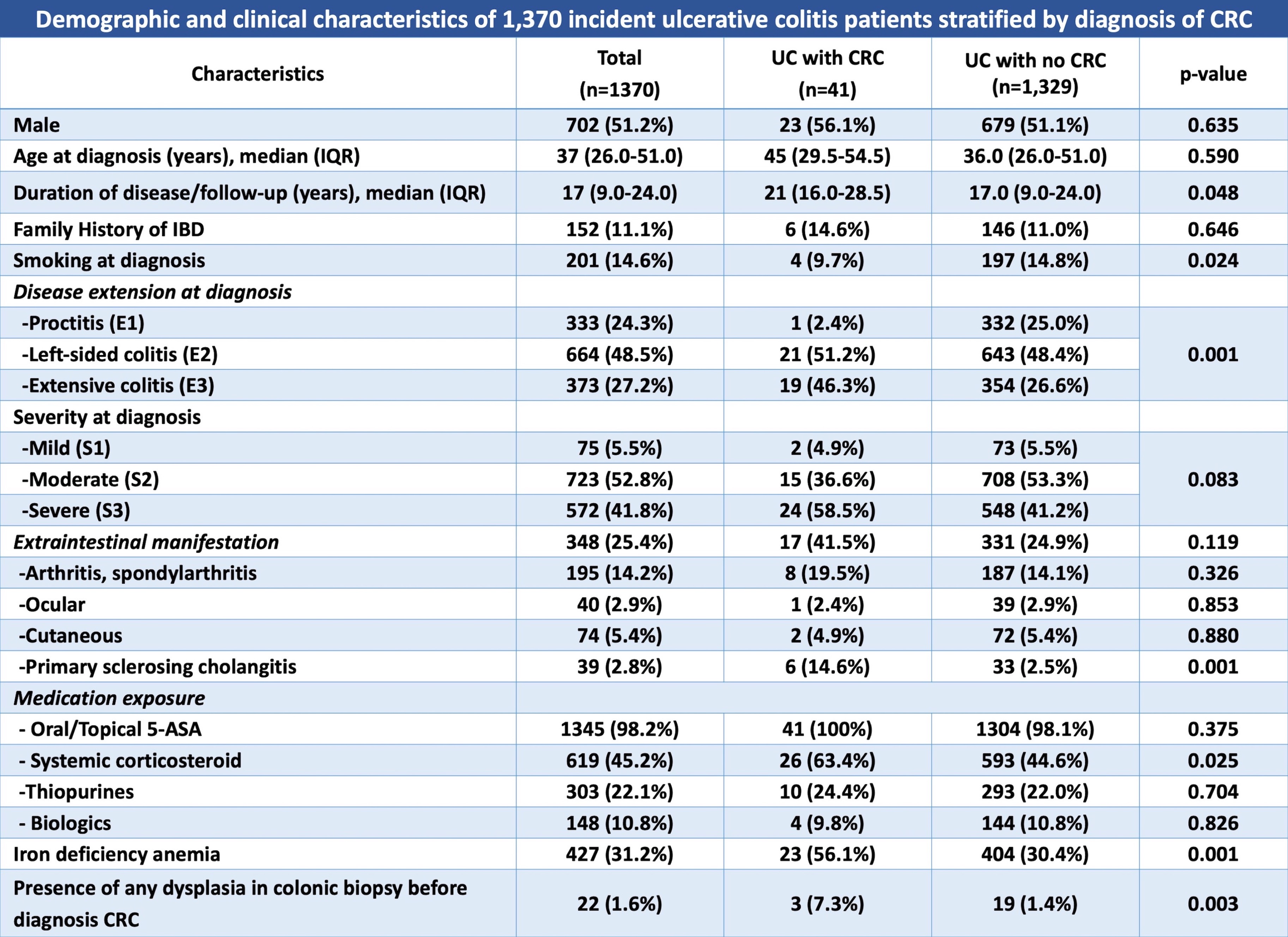

Conclusion
We report an increased CRC risk in UC patients with a standardized incidence ratio of approximately 2 folds, with a stable CRC risk over four decades. Disease extent, co-existing PSC and dysplasia were identified as predictors of CRC.


