P852 predictors of complicated disease course in UC in an administrative database: a nationwide study from the epi-IIRN
Lujan, R.(1)*;Atia, O.(1);Focht, G.(1);Greenfeld, S.(2);Kariv, R.(2);Loewenberg Weisband, Y.(3);Lederman, N.(4);Matz, E.(5);Dotan, I.(6);Turner, D.(1);
(1)Shaare Zedek Medical Center, Juliet Keidan Institute of Pediatric Gastroenterology Hepatology and Nutrition, Jerusalem, Israel;(2)Israel and the Sackler Faculty of Medicine, Maccabi Health Services, Tel Aviv, Israel;(3)Clalit Research Institute, Clalit Health Services, Tel Aviv, Israel;(4)Medical Division, Meuhedet Sick Fund, Tel Aviv, Israel;(5)Leumit Health Services, Leumit Health Services, Tel Aviv, Israel;(6)Rabin Medical Center and the Sackler Faculty of Medicine, Division of Gastroenterology, Petah Tikva, Israel;
Background
There is uncertainty about the ability to predict disease course in UC, often since prediction studies are small and include selected population. We aimed to use a large nationwide cohort to explore predictors of disease course in UC.
Methods
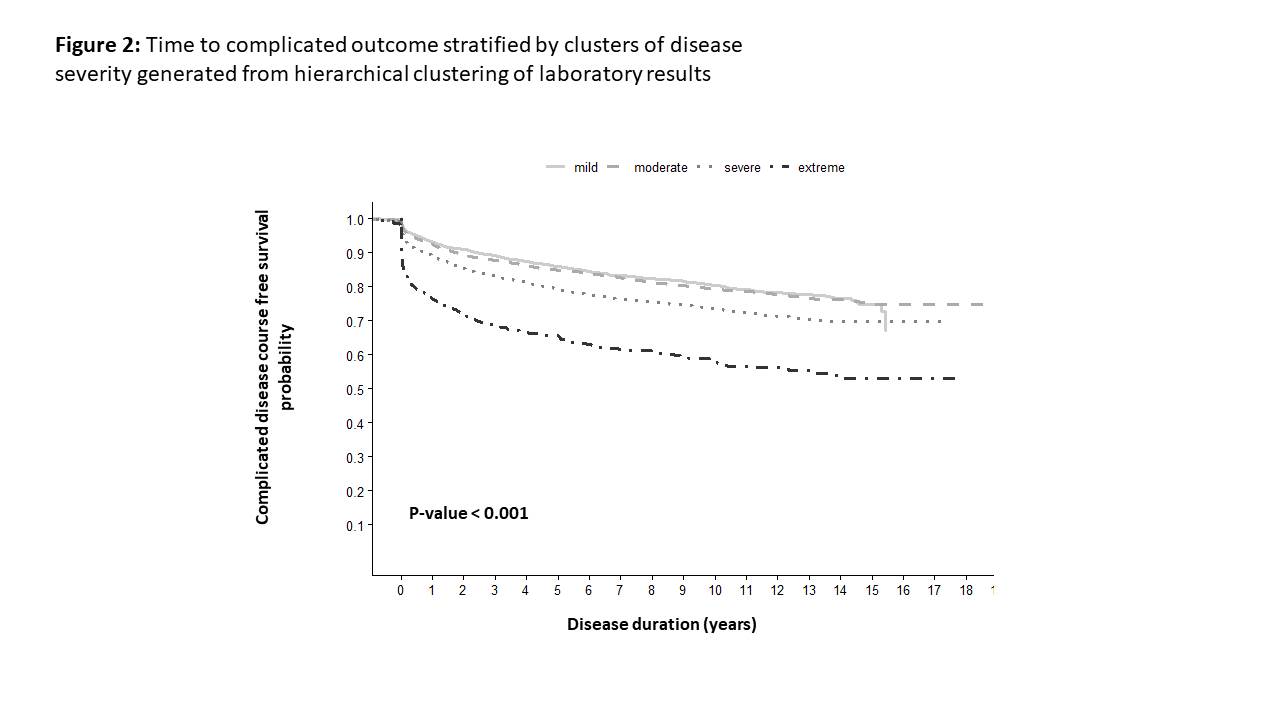
Data of patients diagnosed with UC in the epi-IIRN cohort 2005-2020 were retrieved from the four Israeli Health-Maintenance-Organizations covering 98% of the population. The following potential predictors were explored: demographic data, laboratory results, induction medications, and extra-intestinal manifestations. The primary outcome was complicated disease course defined as colectomy, steroid-dependency, or need for more than one biologic class. Hierarchical clustering categorized disease severity at diagnosis based on available laboratory results into four groups of disease severity (mild, moderate, severe, and extreme).
Results
A total of 15,111 UC patients with 114,208 person-years of follow-up were included, of whom 2,213 (14%) had complicated disease course. The latter was predicted in a Cox multivariable regression model by induction therapy with biologics (HR 3.84 [2.4-6.12]) and severity of laboratory tests prior to diagnosis (HR 1.41 [1.03-1.92]). The use of topical treatment (5-ASA or steroids enema/suppository) as monotherapy was protective with a decreased risk of complicated disease course (compared with untreated, HR 0.5 [0.38-0.63). Younger age of diagnosis (HR of pediatric-onset compared to adult-onset 1.79 [1.48-2.15]) and recent year of diagnosis (HR 1.03 [1-1.04]) were also associated with complicated outcome. Jews had 23% reduced risk of complicated disease course compared with Arabs (HR 0.77 [0.60-0.97]) (Figure 1). Specifically in the laboratory tests, there was a gradual increase in complicated disease amongst the disease severity clusters (p<0.001; Figure 2). 
Conclusion
In this nationwide cohort, complicated disease course was apparent in 14% of patients and predicted by serum laboratory tests and induction therapy with biologics. Jewish ethnicity and topic therapy (reflecting proctitis) were associated with better outcomes.


