P887 Epidemiology of perianal fistulising Crohn’s disease: a systematic literature review
McKay, C.(1)*;Pacis, S.(2);Bolzani, A.(2);Geransar, P.(3);Panés, J.(4);
(1)Takeda Pharmaceuticals USA Inc., Global Evidence & Outcomes - Gastroenterology, Cambridge- MA, United States;(2)Ingress-Health HWM GmbH an affiliate of Cytel Inc., Real World Evidence, Hannover, Germany;(3)Takeda pharmaceuticals International AG, Rare GI, Zurich, Switzerland;(4)Hospital Clínic de Barcelona- IDIBAPS- CIBERehd-, Gastroenterology, Barcelona, Spain;
Background
Complex Crohn’s perianal fistulas (CPF) are a debilitating complication of Crohn’s disease (CD). Data about the epidemiology of complex CPF are limited. This systematic literature review (SLR) aimed to understand the epidemiology of CPF in adult and paediatric CD populations globally.
Methods
Electronic databases (MEDLINE, Embase, EBM Reviews, EconLit) were searched. PICOS-T (population, interventions, comparators, outcomes, study design, time) selection criteria were used to identify relevant studies, and two reviewers independently screened and extracted data. Articles included observational studies with >50 patients published in English from 1 Jan 2015 to 17 Feb 2022. The study was still included if complex CPF was not defined. The NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was used to assess the risk of bias/quality of studies (good, fair or poor). Outcomes of interest were the prevalence and incidence of CPF. Studies reporting epidemiology as an objective were considered primary epidemiology studies. Data were summarized using descriptive statistics.
Results
In total, 140 studies were included, of which most were of good (n=14) or fair (n=98) quality regarding risk of bias. Few studies (n=24) defined complex CPF; hence, outcomes included all types of CPF. An epidemiology outcome was reported in 86 studies (covering all major geographic regions and age groups; Table 1), including 36 population-based studies and 20 primary epidemiology studies. CPF prevalence, reported in 84 studies, varied widely (Table 2). For adult studies (including those not reporting an age range; n=44) and paediatric-only studies (n=15), CPF prevalence (interquartile range) was in the range 1.5–81.0% (10.5–30.1%) and 5.5–47.3% (13.1–19.9%), respectively. Complex CPF prevalence (range) was reported in 18 studies and varied widely (3.4–54.6%); of these, four were primary epidemiology studies (3.4–29.3%). CPF incidence was reported in 15 studies: two studies reported incidence in person-years (PY) as 133.83 per 100 000 PY and 1100 per 100 000 PY. Of studies reporting cumulative CPF incidence at specific timepoints, incidence at 1 year after CD diagnosis was most frequently reported (n=8, range 3.5–50.1%; Table 3).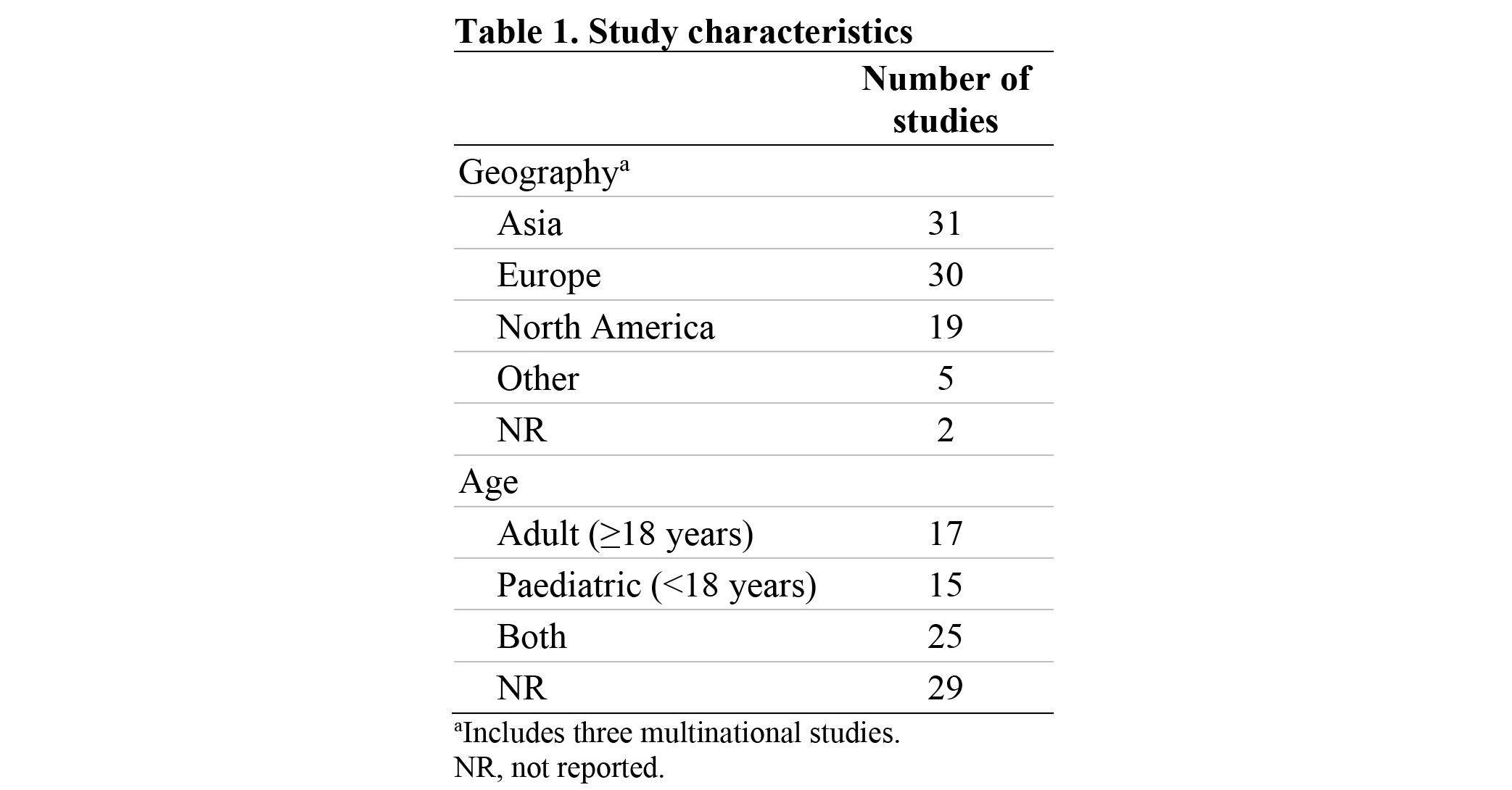


Conclusion
This SLR highlights a wide range in prevalences and incidences of CPF, potentially due to a lack of standardized definitions for CPF alongside a range of reported timepoints. Prevalences were up to 81.0% for CPF and 54.6% for complex CPF, and CPF incidences reached 1100 per 100 000 PY. This SLR demonstrates that understanding the burden of CPF in CD populations globally is challenging and consistent definitions are required to permit cross-study comparisons.
Funding: Takeda Pharmaceuticals USA, Inc.


