P894 Diagnostic yield of routine stool pathogen tests during the relapse of Inflammatory Bowel Disease
Huang, V.(1);Albadrani, A.(1);Alshowair, M.(1)*;
(1)Mount Sinai Hospital - University of Toronto, Gastroenterology, Toronto, Canada;
Background
To make the diagnosis of Inflammatory bowel disease (IBD) flare, it is traditionally necessary to exclude infectious colitis, including bacteria and parasites. Furthermore, Infectious colitis prevalence varies between geographic areas of the world.
It has been a routine clinical practice of sending broad stool testing and cultures to the laboratory before starting targeted therapy for IBD flare. The purpose of this study is to examine the yield of stool testing in adult patients with inflammatory bowel disease flare.
Methods
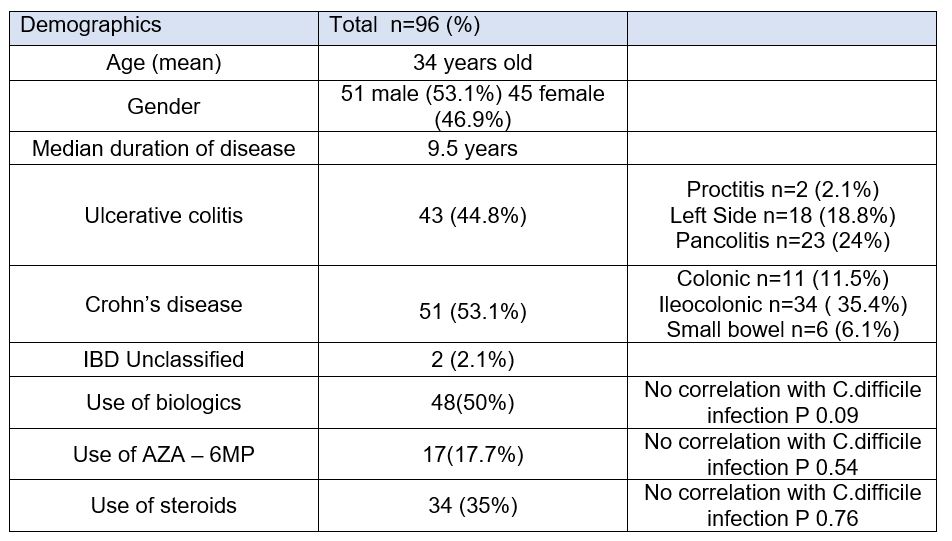
It is a retrospective study. We reviewed the medical records of the admitted patients with IBD flare at Mount Sinai Hospital, Toronto, Canada between October 2018, and August 2019. We used a computer-generated list of patients admitted with a diagnosis of IBD. We excluded patients with no confirmed diagnosis of IBD or admitted for reasons other than IBD flare. A number of variables were recorded, such as the patient's demographics, concurrent and previous IBD therapy, steroid use, presenting symptoms, vital signs, and the results of the initial laboratory investigation
Results
This study included 96 adult patients admitted with IBD flare. A total of ninety-four of our samples were tested for C. difficile at the time of admission. Only 9.4% were positive for C. difficile. Six of them had ulcerative colitis and three had Crohn’s disease.
The percentage of patients evaluated with stool cultures was 86%, while the percentage of patients evaluated for ova and parasites was 51% at the time of patient admission. Only 34% of the population had colonic biopsies stained for Cytomegalovirus (CMV) of which 74% had ulcerative colitis. None of the stool cultures nor CMV tests were positive in our population.
The risk of acquiring C difficile infection was not significantly correlated with the patient's disease phenotype, the biological therapy they were receiving, or their smoking history. In our sample, clinical tests and routine laboratory tests did not predict infectious colitis. The CRP level, as well as the neutrophil and eosinophil counts, were not associated with positive C. difficile infection.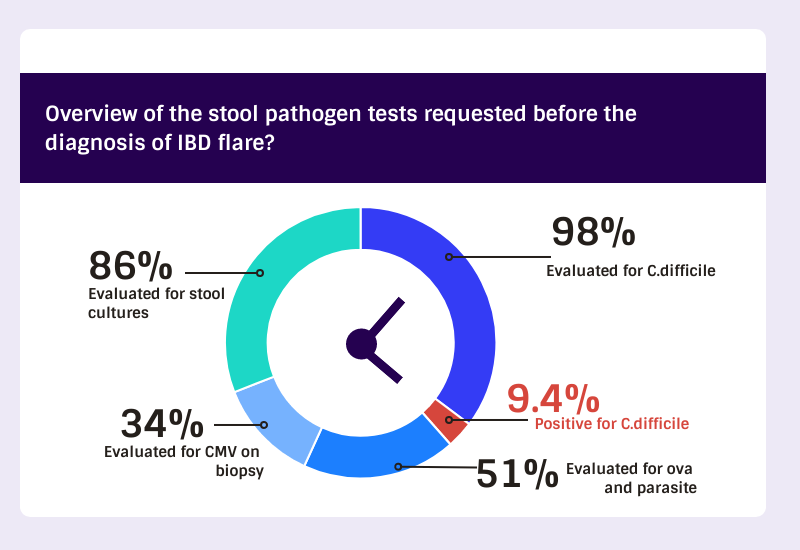
Conclusion
In IBD flare, we did not routinely identify pathogens besides C difficile. Aside from areas where bacterial or parasitic infections are prevalent, routine stool testing with cultures and parasites has a low yield.