Report from IIS Award Winner 2022: Edouard Louis
Edouard Louis, ECCO Member
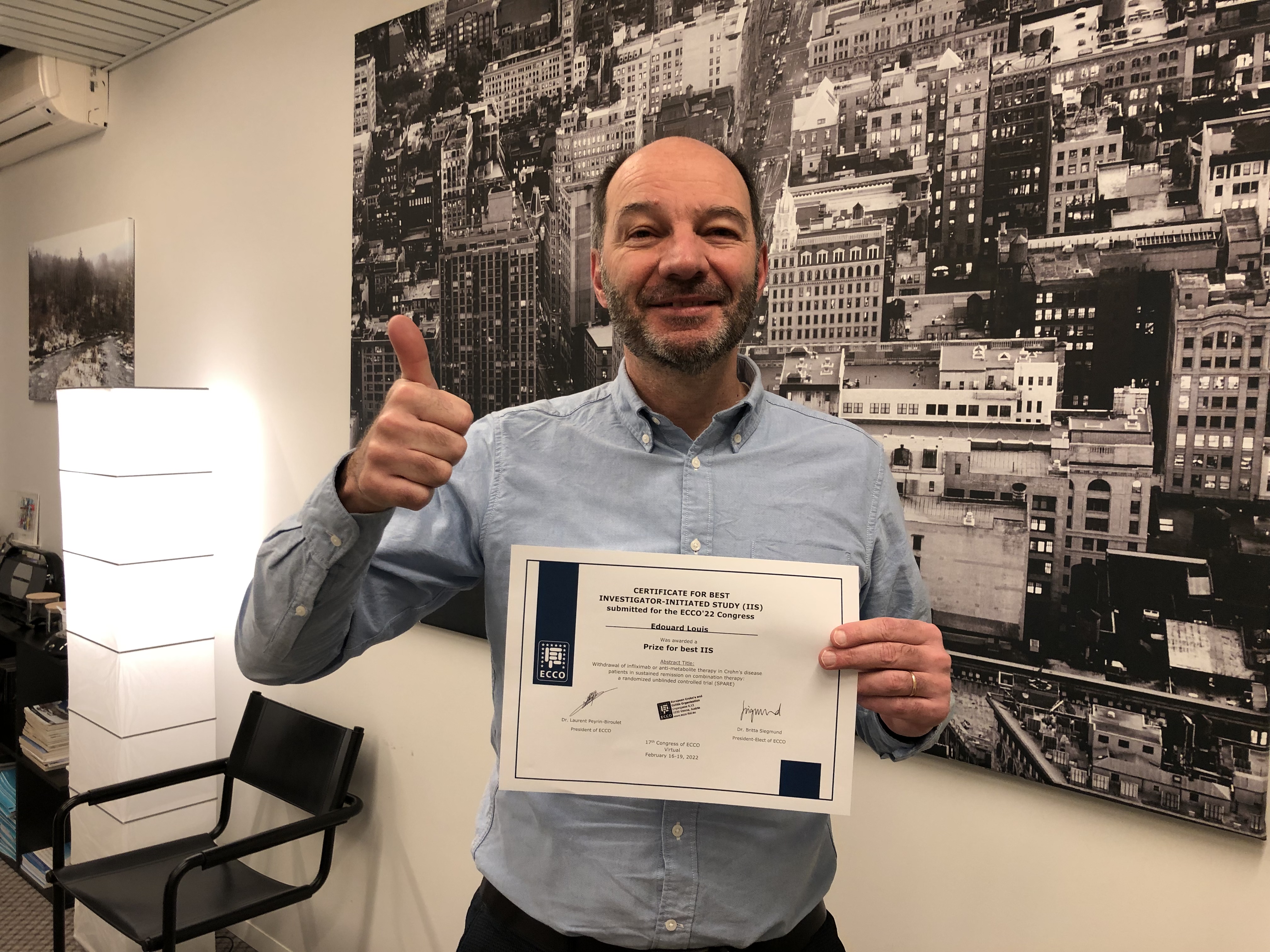 Edouard Louis © Edouard Louis |
The SPARE clinical trial
A treat-to-target strategy and tight disease control may improve outcome in Crohn’s Disease (CD). However, this approach may necessitate long-term use of biological agents and immunosuppression. Combination therapy with anti-TNF and antimetabolite agents is now well established in this context. These drugs may be associated with long-term risks and elevated costs. It is important to establish whether treatment de-escalation, once deep remission has been achieved, is feasible and whether this strategy may improve safety profile and costs without jeopardising disease control.
Infliximab (IFX) withdrawal in patients with CD in sustained steroid-free remission has been associated in uncontrolled studies with an increased risk of relapse of around 50% over 2 years. However, these studies also suggest that remission can usually be recaptured by resuming the treatment, suggesting that no harm would be generated for the patient. Previous uncontrolled data suggest that withdrawal of antimetabolite therapy in patients who have achieved durable remission on combination therapy may not alter relapse rates.
SPARE was a randomised, controlled, non-blinded multicentre trial (64 sites in Europe and Australia) involving CD patients in sustained steroid-free remission for at least 6 months who had received combination therapy with IFX and an antimetabolite (thiopurine or methotrexate) for at least 8 months. Patients were randomised into three arms: continuing combination therapy (arm A), stopping IFX (arm B) and stopping antimetabolite (arm C). In the event of relapse, patients were retreated according to a pre-defined scheme. The co-primary endpoints were the relapse rate and mean time spent in remission over 2 years.
Out of 254 screened patients, 211 were randomised and 207 were involved in the final analysis: 67 randomised to arm A, 71 to arm B and 69 to arm C. The two-year relapse rates were 14% (95% CI: 4%–23%) in arm A, 36% (95% CI: 24%–47%) in arm B and 10% (95% CI: 2%–18%) in arm C (p=0.003 arm B vs arm A and =0.0004 arm B vs arm C). Twenty-eight patients in relapse were retreated per protocol. Remission was achieved in 1/2 retreated patients in arm A, 22/23 in arm B and 2/3 in arm C. The mean time spent in remission over 2 years was 1.91 years (95% CI: 1.83–1.99), 1.89 years (95% CI: 1.82–1.97) and 1.93 years (95% CI: 1.87–2.00) in arms A, B and C, respectively.
This randomised controlled study confirmed the increased risk of relapse in CD patients associated with stopping IFX. Almost all patients regained remission when resuming the treatment and only a minimal decrease in the time spent in remission was observed. Antimetabolite withdrawal was not associated with an increased risk of either relapse or drug immunogenicity.
Treatment de-escalation by withdrawing IFX may be contemplated in CD patients in sustained steroid-free remission. This approach should be tailored to the individual patient to improve the benefit/risk ratio of the treatment. Antimetabolite withdrawal does not appear to increase relapse rates or anti-drug antibody formation in those continuing on IFX monotherapy.


