Y-ECCO Interview corner: Ailsa Hart and Willem Bemelman
Nuha Yassin, Y-ECCO Chair
 Nuha Yassin © ECCO |
Dear Y-ECCO Friends,
In our series of Y-ECCO corner interviews, we are adding a new flavour for 2018 by conducting a tandem interview with the IBD giants. Today, I am delighted to be joined by Ailsa Hart and Willem Bemelman, who are respectively a leading gastroenterologist and leading surgeon in the world of IBD. We have all heard them give tandem talks and look forward to finding out more about them in this tandem interview. Many thanks for agreeing to be interviewed, Ailsa and Willem. We’ll ask you similar questions and see if the answers are similar or different.
Nuha Yassin
Y-ECCO Interview Corner Coordinator
 Ailsa Hart © ECCO Ailsa Hart © ECCO |
Can we start the interview by asking Ailsa, who is Ailsa Hart?
Ailsa: That’s a very good question to start with. Ailsa Hart started her life in Durham, which is in the north east of England, as the younger daughter to two wonderful parents. My mother was a doctor (Dr. Hart), and my grandfather was also a doctor (Dr. Hart). So I’m the third generation of Doctor Harts, and that’s what I like to think of when asked who I am. I start from Durham with a very happy family, with a sister and very happy parents. I am mum to Ollie and Edward and wife to Andy, that is actually who I am. What gets me up in the morning is actually to look after that unit. So, although I have a really good job which I really enjoy, what really defines me and gets me going in the morning is looking after my own little family unit.
Did your family inspire you or push you to become a doctor?
Ailsa: Another good question. Very genuinely I can say that I was not in any way pushed. I was very much Inspired. It became clearer that I was better at science subjects when I was young, so I did science A-Levels and wanted to do something with the science A-Levels as a long career, and I think that’s when it became clear to me that medicine was for me. There is no doubt that I did get inspiration from the two generations above me. My grandfather was a fascinating character who started his life in literally the very poorest part of Glasgow. He was a very good football player who played for the Rangers football club, and this enabled him to pay his way through medical school. He was always a very inspiring character in my life. And of course, my mum was always an inspiration. I do remember my grandfather telling me that if you do medicine, you will never make a fortune but you will never starve. That seemed to tick quite a few boxes really because you wouldn’t make a fortune but you would have security and great job satisfaction. The stories my grandfather used to tell me about his early years in Glasgow and the stories my mother used to tell me were inspiring, and I’m sure that’s why I ended up falling into medicine.
 Willem Bemelman © ECCO Willem Bemelman © ECCO |
Willem Bemelman, thank you for talking to me today. Similarly, may I ask you to forget Professor Bemelman for a minute and tell me who is Willem?
Can you talk me through your career? How did you get into medicine/surgery?
Willem: My father was a technical engineer, so he went to Delph, one of the most important universities in the Netherlands, and was a very smart guy. He always admired the medical profession and that stimulated my sister and me to become doctors, although in Delph they always said if you’re not smart enough to study engineering then you could always study medicine. So on the one hand, my dad admired the medical profession, but on the other, he said it was easy to get into. My father was also very handy at home, restoring the house and building new things and working on all sorts of DIY, in which I helped him out. I loved working with my hands and was good at it, so for me it was logical that I would choose surgery and work with my hands. So I always joke that the ECCO Interaction party should be called “Hands and Minds” rather than “Hearts and Minds”.
From the first surgical lecture in medical school, I knew I wanted to be a surgeon. That helped me focus on building my portfolio towards a surgical career, as at the time only 17 young doctors were allowed to go into surgery. It was very competitive. I was very focussed. I taught anatomy for 3 years during medical school, and did my PhD in a surgical topic before graduation. I also studied for the USMLE (American exam) to widen my opportunities and go into surgery in the US if I was unable to do so in the Netherlands. Fortunately I was one of the 17 chosen ones who were able to get into surgery in the Netherlands. I arranged with my clinical partner to stay for 4 years in the academic hospital whilst training and to spend the other 2 years in the non-academic teaching hospital. I had a scientific profile at the AMC, and gained very good surgical experience in a busy unit. I was the first to be taught how to do laparoscopic procedures as a chief resident. That meant that when I was oncall I did all of the surgical procedures. So at the end of my surgical training I had vast experience in minimally invasive and open general GI surgery. There were no consultant positions available at the AMC when I graduated, and at that time fellowships did not exist, so I went almost immediately into a consultant position at Leiden University, just 6 months after finishing my surgical training. I was in charge of the benign GI surgery when I started in Leiden, which included IBD and other GI conditions. I had an annual caseload of 600 procedures, which is crazily busy. At that time, laparoscopic surgery for colorectal cancer was restricted by the fact that port-site metastases were seen. But such restrictions were not in place for benign disease, so I started to establish and expand my laparoscopic experience in IBD and was able to establish an IBD portfolio doing laparoscopic ileocolic resections, subtotal colectomies and pouch surgery. This experience started from my first year of being a consultant.
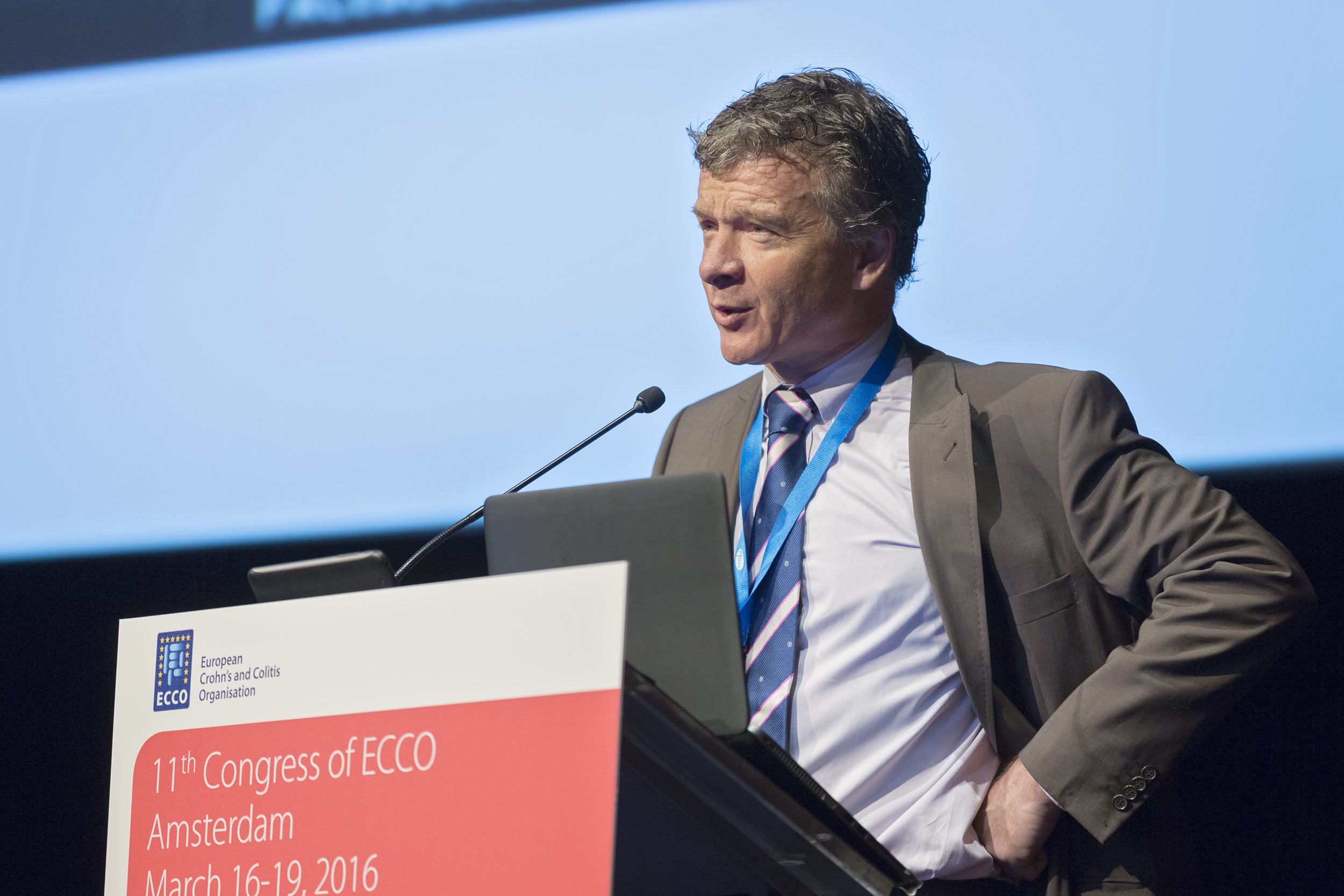 Willem Bemelman at the 5th S-ECCO IBD Masterclass at ECCO'16, Amsterdam © ECCO Willem Bemelman at the 5th S-ECCO IBD Masterclass at ECCO'16, Amsterdam © ECCO |
I visited the Cleveland clinic for 2 weeks before I went to Leiden and I watched laparoscopic ileocolic resections over there and thought to myself, I can do that in the Netherlands. I expanded my laparoscopic colorectal experience from using hand ports initially to pure laparoscopic resections and built a large portfolio of experience. I currently use hand port-assisted laparoscopic surgery for emergency work and for extensive fistulising Crohn’s Disease, very specific indications.
After 4 years of high-volume IBD and other laparoscopic GI surgery at Leiden, I received a phone call from one of the professors at the AMC informing me that they wanted me back. I didn’t hesitate at all in deciding to go back to the AMC as I had always wanted to work there and it was my first love. I was appointed at the AMC to implement laparoscopic surgery in general and I did so for all GI procedures until more subspecialist appointments were made and I was able to focus once again on IBD and colorectal surgery.
Laparoscopic surgery was new at the time, and as with everything new, there were a lot of dinosaurs sitting waiting for any negative mishaps to occur so that they could stop the laparoscopic practice. The way to counteract that and continue doing laparoscopic surgery was to immediately start doing clinical trials. As long as a practice or a procedure was within a clinical trial, then it had no restrictions from governing boards within the hospital.
I immediately set up a clinical trial looking at laparoscopic vs open ileocolic resection (the LapTop study), and I also set up the only study looking at laparoscopic vs open pouch surgery, so then it was OK to do laparoscopic surgery as it was within a clinical trial.
I also joined the sigma study (for diverticulitis) and the llama study looking at laparoscopic closure of peptic ulcer perforations. Therefore, most of the laparoscopic work was within a trial and met no resistance from the rest of the group.
 Willem Bemelman at the S-ECCO IBD Masterclass Willem Bemelman at the S-ECCO IBD Masterclass at ECCO'13, Vienna © ECCO |
Over time we established laparoscopic and minimally invasive work in all aspects of abdominal surgery and my work opened up the door at the AMC for the establishment of minimally invasive surgery.
So, my love for IBD goes back a long time, to my junior surgical training and the high-volume units in which I worked at both Leiden and the AMC. I was able to establish my laparoscopic IBD career very safely, going through my initial learning curve at Leiden and then expanding my knowledge at the AMC. I then introduced laparoscopic work in colon and rectal cancer surgery and was involved in many trials and also introduced re-do work and salvage surgery.
Times are now slightly different with training. Surgical training used to take 6 years, but now the trainees are expected to take up a 2-year fellowship and continue training through mentorship, after the 8 years post-graduation. I would have loved to have gone abroad for half a year or a year after graduation, but such a course of action was not so common back then as fellowships are nowadays. And on the other hand, in my time it was not that difficult to go through training and get a job as there were only 17 people getting into surgery. Now there are the limited working hours, whereas in the past there were no limits to training times.
I guess surgical training is different now and there are some differences in each country. In the UK the minimum time any surgeon can spend in training post-graduation is 10 years, and that’s without PhDs or fellowships. Do you think fellowships are important nowadays? And can one gain any experience from observerships?
Willem: I think fellowships are very important so that trainees can go to different units and learn how things are done differently and avoid getting set in doing things one way. Observerships are also very important as they teach skills that are much more important than hands-on craft skills. One assumes that if a surgical trainee reaches the end of their training successfully, they can actually operate. What observerships teach are the decision-making skills in complex cases and the management skills. But observerships should not be too long: a maximum of 4 weeks, otherwise things risk becoming repetitive. Hands-on fellowships can be difficult outside one's own country due to language barriers within Europe. It would be useful if a trainee were able to do a 6- or 12-month fellowship if their training has failed to provide them with exposure to the variety of surgical procedures and how to deal with them. With troubleshooting and decision making during surgery, it helps a lot if you have seen some surgeons in difficult situations solving similar problems.
 Willem Bemelman at the 6th S-ECCO IBD Masterclass at ECCO'17, Barcelona © ECCO Willem Bemelman at the 6th S-ECCO IBD Masterclass at ECCO'17, Barcelona © ECCO |
So, when we look at you and other surgeons, what kind of skills do you think are required? Are surgeons meant to be scientists and researchers and clinicians, or should they just stick to operating?
Willem: I think it depends on the person's skill mix. Of course we need surgeons who only operate. Surgeons in normal, non-academic teaching hospitals who don't have the time to do science can do a lot of education, which is very important. They can also be in management positions within their hospital and national societies. They can also contribute to science by participating in clinical trials and adding data from their units. So it’s a question of what's in one's nature, what one likes doing and is skilled to do. The interesting thing with my job is that it is so diverse that if I have a bad day, for example a bad complication, there is likely to be something on the same day that cheers me up again, such as when I give a nice lecture to the students and see how much they appreciate it. So I normally find positive things in my day owing to the diversity and variety of things: it is very rarely that there are no positive things in a single day. And even if a day has been absolutely bad, I just get on my bike at home for a while, which releases all the endorphins in my body, stimulating me and lifting my spirits.
That's great, thank you Willem. Now going back to Ailsa: being an Oxford trainee, and a very bright student, were you always successful throughout your schooling and training, or have you had some tough times and challenges, like most people? Y-ECCOs look up to successful giants like you and Willem and wonder if a normal trainee can achieve as much as you have, or whether you're both superhumans who have never been on a roller-coaster ride?
Ailsa: For sure it is a roller-coaster at times, but I think one thing I’ve always done is to have a very, very strong work ethic. I’ve always tried hard and I’ve always worked hard. That’s probably been the passport to where I’ve got to. I’ve consistently and persistently, over my life, worked hard and given it my best. So even when there have been the drops, one must pick up, work hard, be dedicated and keep focussing on the goals and the aims.
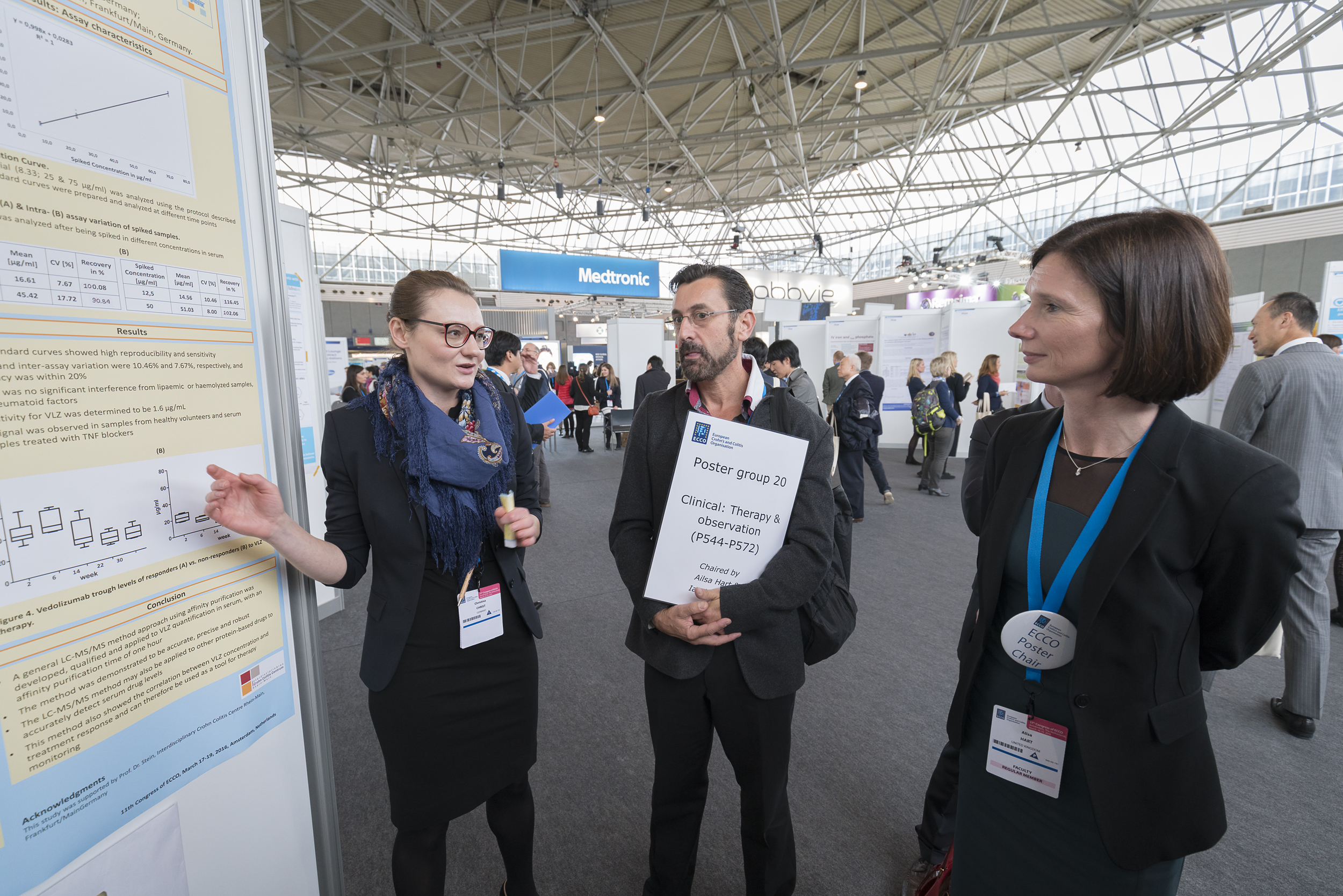 Ailsa Hart at ECCO'16, Amsterdam © ECCO Ailsa Hart at ECCO'16, Amsterdam © ECCO |
Through school I was pretty successful, but I remember going from Durham to Oxford University feeling like an utter fish out of water, wondering how I could ever fit in with all of these super-clever people. It all just felt a bit different. It was the first time I had ever been away from home, and that was a deep breath. For the first time at university, and for the first moment in my life, I felt that I was nowhere near good enough, and that feeling was just not me at all. But gradually it became clear that it was absolutely fine and I was absolutely fine there and did jolly well.
Has it always been medicine, or were you just interested in sciences? And why have you chosen to specialise in gastroenterology and IBD?
Ailsa: It has always been medicine for me. It’s the people. That’s what’s always been a big driver for me. Doing science and medicine without patients, without actually seeing why you’re doing it, would never tick my boxes, and would never appeal.
As for gastroenterology, it is quite simple. When I was a medical student I worked for Derek Jewel in Oxford, who was obviously doing a lot of the IBD research at the time in the UK. He had a couple of research fellows at the time, Jack Saktangi and Miles Parkes, and I can genuinely say they were a part of why I did gastroenterology because they were doing research with Derek Jewel at the time and they made gastroenterology seem really cool. I thought there was a phenotype of people in any speciality, and I looked around at the other specialities like neurology or cardiology and then looked at gastroenterology and I thought I was more like that. Gastroenterologists are a bit more down to earth, a bit more practical and quite fun, and that’s what attracted me to gastroenterology.
 Ailsa Hart at ECCO'18, Vienna © ECCO Ailsa Hart at ECCO'18, Vienna © ECCO |
My next major interaction which also pushed me that way was when I went to St Mark’s Hospital in London, as my first SHO (senior house officer) job. So I was a very junior doctor in 1996. I had literally just done my surgical house officer job in Southampton and arrived and walked through the doors of St Mark’s and realised it was quite a strange place. It was all a bit different. I met Michael Kamm at the time, and he very much took me under his wing and thought I had potential; he is another key figure in my life who recognised I had the potential and nurtured me towards gastroenterology and IBD. St Mark’s had a family atmosphere right from the word go, I remember it so clearly still. There was something that was a bit of a draw to the place.
Let’s talk about phenotypes, as you have mentioned it, Ailsa. Do you think there are similarities between gastroenterologists and colorectal surgeons? Or differences for that matter?
Ailsa: I think there are similarities and differences, but I think there are more similarities between gastroenterologists and surgeons than we think. If I reflect back on the early days of St Mark’s when I arrived there, there were two camps, and a clear division between gastroenterologists and surgeons. This was 20 years ago, though, in 1996, and I have since seen a much greater blending of colorectal surgeons and gastroenterologists over time, and it feels like a much more joined up group now. There are very practical differences. Surgeons are fantastic with their hands and doing things, and endoscopists likewise. So different things are brought to the table.
What about the personalities? Are surgeons and gastroenterologists both type A personalities? Do gastroenterologists secretly want to be surgeons? After all, gastroenterology is also a craft speciality with advanced endoscopic skills etc.
Ailsa: I think probably both surgeons and gastroenterologists have type A personalities. There is a drive on both sides. I have never wanted to be a surgeon: it would never light my fire doing the surgical bit of IBD. There are advanced endoscopists who work very closely with surgeons and do combined procedures together, and depending which part of the world you live in, some skills are done by one or the other or there is more combined work. I think one should recognise one’s interest and skill mix and go with that.
Do you think one needs to be a certain type of personality to be successful?
Ailsa: It depends how you define success. Success is quite a personal thing actually. Objectively people might perceive someone to be successful and another not to be, but there’s also a personal attainment of goals, which is probably the more true definition of success. So, colleagues in smaller hospitals, any of them could do what I do, if they had chosen to. They are very successful and good at attaining success in what they do, maybe innately and from a personal level. So, how you objectify something like success is quite interesting, and that’s all perceptual. It could be defined by objectively defined things such as grants or papers or major collaborations, or by other academic things you can actually benchmark. But, then again, even with that, what is success?
So how does Ailsa Hart define success?
Ailsa: I think it is more on a personal level, because for me, success is not just success in my work life, it also has to be a personal feeling of success in my family and personal life, otherwise I would not feel successful. If one of the things was failing dramatically, I personally would not be defining myself as successful. If I was the most cited gastroenterologist in the world but had a miserable personal life, I would not feel that I was successful. Success has to have things somewhere in balance, otherwise it utterly unravels into a hollow existence.
 Ailsa Hart at ECCO'15, Barcelona © ECCO Ailsa Hart at ECCO'15, Barcelona © ECCO |
You have a beautiful family and a successful career, how do you balance it all?
Ailsa: My family are always a big priority for me. I am quite low down on my priority list. My family and my work are high up. I am very fortunate that I have a wonderful husband who is very hands-on and I have two boys, so actually a father figure is particularly important as the boys get older. I have always pushed myself even when I’m exhausted to make sure I’m absolutely giving what I can to my kids and my husband. Probably the only time that I’m relaxing is when I’m horizontal with my eyes closed, otherwise I am always giving my time to my family or my work. It takes a lot of effort to relax and come back fresh the next day. Relaxing with my boys is how I do it. When you’re with your kids you have to empty your mind and everything that’s being going on during the day, divorce yourself from your work and give the kids undivided attention. You’re completely focussed on whatever is in their life and their heads at the moment, and that’s very relaxing. There’s nothing I like more than watching my boys play sports at the weekend. Any time with them is important time. It might not be perceived as relaxing for some other people, but for me, it’s very different from the work side of things and is very relaxing. There are two units that I look after, the IBD unit and work-related matters and the family unit. The two units are quite separate and it’s a really momentary time when I leave work and am on my way home. It really feels like it's a separate life, and a complete brain switch and you focus on family as soon as you leave work. Andy and I met when we were at school and he's doing well and we all need each other. I always have photos of the boys by my bed even when travelling for work. Obviously one thinks of work matters, but it’s a matter of balance.
Talking about family, we are now back with Willem. Do you get to see much of your family? How do you balance things out? Do you ever take work home with you?
Willem: I also have gorgeous boys, but they are now teenagers. It was different when they were younger and needed more attention. Now, if I’m lucky when I come home they might say 'Hi dad' and then they go back to doing their homework or watching television or gaming. It is really enjoyable to meet them at the dinner table for maybe 15 minutes and see them walking around in the house. At this age it's probably more the fact that I am present rather than in-depth communication. When the kids were younger, my wife (who's also a surgeon) and I both worked. So we had a very good structure of how to take care of the kids and had enlisted the help of a good network, including the grandmother. It worked really well during the week, and at the weekend we looked after the kids ourselves.
 Willem Bemelman at ECCO'14, Copenhagen © ECCO Willem Bemelman at ECCO'14, Copenhagen © ECCO |
I think your family will be happy if you're also happy in your work. I also put a lot of effort into having protected family times and going on family holidays and really enjoyed playing sports with my sons and also learning something from them. We enjoy doing many activities together like water skiing and diving, and now every Sunday the whole family, including my wife, are learning kick-boxing. It isn't about the activity, it’s about spending time together away from work.
Work does have to come home though. After dinner I do some work till 11 p.m., but then I stop and do something else relaxing. But mentally, I do take my patients with me, and I think any good, caring doctor would do the same. This is particularly true if I’m worried about a major complication, as there are four colorectal surgeons in our unit and we are always sorting out our own colorectal group patients and the potential complications. So although officially the oncall is 1:10, we are in fact oncall 1:4 so that we can look after our colorectal patients.
So, I’ll ask you the same phenotype question I’ve just asked Ailsa. Do you think there's a specific personality that is attracted to surgery or gastroenterology? Do we have to be type A personalities?
Willem: I think we are the type that combines hands and minds. We are curious, innovative and direct. We are good at acute problem solving and I think we are a very positive group of specialists. We have to be very positive, otherwise we would not be able to cope with the immediate stresses and potential complications of a technically challenging operation.
I don't think surgeons have to be type A personalities. But we do have to be more outspoken than other medical colleagues as we are usually in a minority, and the other groups are bigger and mostly have more money. So we have to do our best to stand up and get our voices heard. It is in our nature, it does come with the surgical nature to be able to speak up for your patients.
This takes me to ECCO, may I ask both of you, Ailsa and Willem, how did you get involved in ECCO and what does it mean to you? We'll start with Willem: isn't this a gastroenterology society?
Willem: It all started with my deep interest in IBD. I love working together with gastroenterologists as we really need the multidisciplinary approach when dealing with IBD. Gastroenterologists can show me what they do, and I can show them what I can do, such as the results of minimally invasive procedures.
 Willem Bemelman at ECCO'14, Copenhagen © ECCO Willem Bemelman at ECCO'14, Copenhagen © ECCO |
I then discovered that ECCO was beginning to have a scientific and educational platform for the multidisciplinary management of IBD patients. The challenge for me, and also for André D'Hoore, was to get into ECCO, as when it first started it was completely dominated by gastroenterologists, who completely embraced us and were welcoming yet somewhat afraid of the surgical interference. With the support of the various stakeholders in IBD, we were able to create the Surgeons of ECCO Committee (S-ECCO). We had the support of the gastroenterologists with whom we worked. They realised it was a good idea to have an S-ECCO Committee as we all work so closely with each other, and that worked out very well over time. I think it was in Prague that André D'Hoore and I held a meeting some time ago discussing the formation of the S-ECCO Committee, and our proposal was welcomed by the Governing Board. We became a solid group of core S-ECCO Members who work well together, organise educational programmes, collaborate on cohort studies and, most importantly, have fun together as a group of friends. More people are joining ECCO and S-ECCO, and we would like to encourage more young people to get involved and to speak at the various sessions, to get some exposure and to have fun with the S-ECCO and ECCO Family. We have grown from 80 initial participants in the S-ECCO Masterclass to 250 and the Masterclass is completely sold out.
How did Ailsa first get involved in ECCO?
Ailsa: The first ECCO Congress that I went to was probably during my research time, but I have been to every single one since. I haven't missed a single one. But I remember getting more involved when I was asked to give a talk at ClinCom meetings, and then some very welcoming members invited me to apply for a position within ClinCom, which I did. I joined with a lovely group, with Filip and Laurent, and that was a really nice time. I felt really embraced by the ECCO Family and really enjoyed my time on ClinCom. One of the big gaps I saw was that the research nurses sometimes felt like a fish out of water. Nurses had N-ECCO and the other clinicians each had their group, but the research nurses needed a network. I felt that ECCO could have a role in addressing this need, helping researchers and research nurses to get together and share information. So I set up the School for Clinical Trialists, which was a big success that sprouted from my ClinCom experience. Then one day I received a call from Julian Panes asking me if I would consider being on the Governing Board, and there was a pause, and then he said as Treasurer, at which point I think I laughed, as I could hardly manage my own piggy bank. It became apparent that it was a very serious proposal. I think I had a discussion with the amazing ECCO Team, who were very helpful. I must admit that the ECCO Office Team are the definition of organisation, functionality, affability and efficiency and I am truly honoured to work with them. It has been a very sharp learning curve but I'm enjoying my new role and really pleased to be working in such an amazing environment with great people. It’s wonderful.
What about you Willem, what does the position of Secretary for ECCO mean to you?
Willem: I think the position of Secretary is one of the most important positions in ECCO because the role of the Secretary is to be involved in and know about all ECCO Activities and to report back to the Governing Board about them. I will be able to give feedback on all the activities and to provide a surgical viewpoint on them.
 Willem Bemelman at ECCO'18, Vienna © ECCO Willem Bemelman at ECCO'18, Vienna © ECCO |
This is a brand new thing in the ECCO Structure and I am delighted to have had the support of the ECCO Members in taking on such a position. I will be able to check that the multidisciplinary approach to the management of IBD patients is reflected within the ECCO Committees. I would be very much in favour of more integration between the different Committees; for instance, I think it is important to have an IBD gastroenterologist in S-ECCO, and other similar integrations. The other thing I find important is the liaison between ECCO and other societies. ECCO is a European society with a global impact. And I think we can improve on the communication between ECCO and other societies, particularly the surgical societies, which play an important role in IBD management. We need more integration within ECCO and with other societies and more multidisciplinary core programme sessions.
And a final question to both giants: Has ECCO affected your career trajectory, and what's your advice to Y-ECCOs?
Ailsa: It is really important to get involved and come and present your work at ECCO. It isn't just about being part of the committees, it’s about the interaction with like-minded colleagues and seniors who are interested in IBD, meeting new people and forging collaborations. One of the real strengths of ECCO is that it keeps limiting the amount of time that any one person receives exposure, and welcomes new faces. There are so many good people, all of whom will bring something new and fresh. Other societies have stuck with the same old faces, which can be off-putting, but ECCO is very welcoming to anyone who chooses to be part of the society. Y-ECCOs who are keen and would like to take part can seek out the many opportunities as well as mentorship from senior clinicians, who would love to see Y-ECCOs succeed as they are the future leaders. Being a productive researcher and being a good clinician requires hard work. The hardest part is the first rung of the ladder, but once you're over that step, the gaps become less wide and it becomes easier, and forging collaborations certainly helps. That's why ECCO is so important, as it is a welcoming family of experts.
Willem: I agree with Ailsa, ECCO has made me really enjoy my work a lot more. I find ECCO to be a very powerful and very organised society. There is a lot of positive energy and a lot of challenges, particularly with respect to integration between the different subcommittees. We need a complete reflection of how we work in an IBD unit and we need Y-ECCOs to be involved and to take things forward in the future. We need to move and look out of the different boxes and truly come together as key members. ECCO offers a lot of opportunities which Y-ECCOs should get involved with. In order to succeed in their career, Y-ECCOs need to look out for these opportunities and work hard. They will subsequently reap the rewards and enjoy the results of working together with different groups on various projects within ECCO and learning from each other.
 ECCO Governing Board at ECCO'18, Vienna © ECCO ECCO Governing Board at ECCO'18, Vienna © ECCO |
Ailsa Hart and Willem Bemelman, thank you ever so much for letting us look into your careers and for your thoughts. Your pearls of wisdom will be passed on. I have thoroughly enjoyed talking to you both and have learnt a lot, and I hope my fellow Y-ECCOs have, too.
Please contact the ECCO Office for any interview suggestions and interact with Y-ECCO on twitter @Y_ECCO_IBD.


