Thrombosis in Paediatric IBD
Richard Hansen, P-ECCO Member
 Richard Hansen Richard Hansen© ECCO |
The risk of thrombosis in paediatric IBD has become a hot topic in recent months, prompted by the publication of two impactful papers in Journal of Crohn’s and Colitis [1, 2]. Kuenzig and colleagues presented a large Canadian population-based study which described a vastly increased thrombosis rate in children with IBD compared to the normal population: the 5-year incidence was 31.2 per 10,000 person-years among children with IBD versus 0.8 per 10,000 person-years among children without IBD (95% confidence intervals 23.7–41.0 and 0.4–1.7, respectively) [1].
This rate was also around three times higher than that suggested by previously published epidemiological data [3] and was highest in the first year after diagnosis. Aardoom, Klomberg and colleagues offered a distinct but highly complementary paper derived from a 30-country safety registry collaboration caring for ~25,000 children with IBD [2]. In this work, the authors described 20 patient episodes of venous thrombosis, of which 50% involved cerebral sinus venous thrombosis, and reported an overall mortality of 10% (admittedly, with a natural selection bias towards reporting of more severe disease).
Use of heparin thromboprophylaxis for venous thrombosis has long been established practice in adult inpatient IBD care but recommendations for similar treatment in children have been scant. One paediatric-specific guideline published jointly by ECCO and the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) proposed thromboprophylaxis in children with Acute Severe Colitis with one or more additional risk factors and dependent on the child’s age [4]. Until this year, this was the only formal guidance advocating use of thromboprophylaxis in children and so no other groups warranted consideration of this therapy.
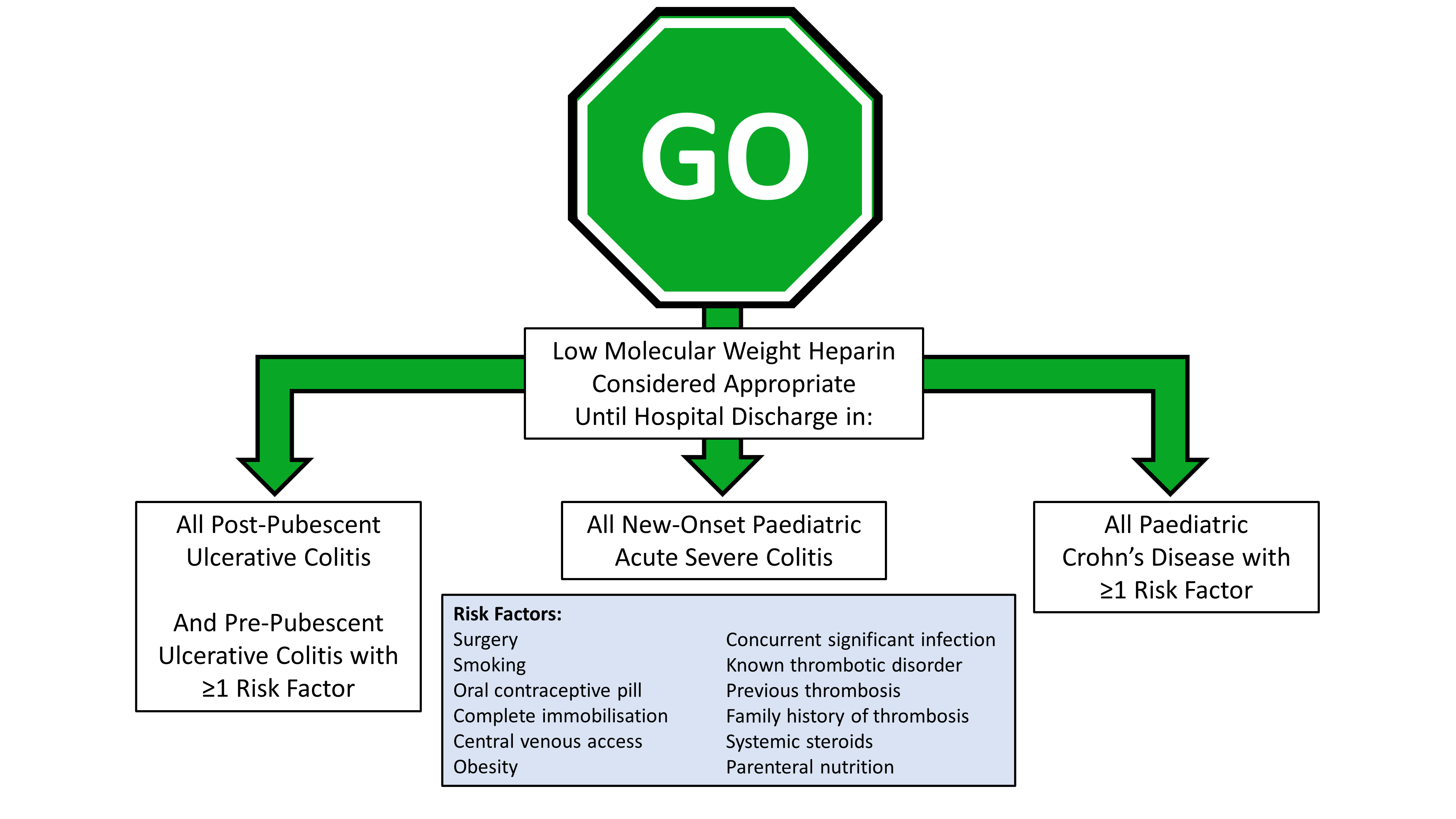
The advent of the COVID-19 pandemic led to widespread and rapid shifts in clinical practice. There was also, naturally, additional concern early on, when little was known about the impact of the virus on immunocompromised patients. This led directly to two RAND panel reviews of existing guidance for the management of Acute Severe Colitis in both adults and children [5, 6], both of which largely supported existing management strategies and the requirement for steroids and additional immunosuppression. RAND panels are a long-established method of assessing and reporting expert opinion when evidence is limited and so were naturally helpful in this period of COVID-associated uncertainty. Somewhat surprisingly, the paediatric RAND panel recommended in favour of thromboprophylaxis in all patients treated for Acute Severe Colitis, irrespective of COVID status [6]. This seemed at odds with the existing recommendations from ECCO/ESPGHAN [4], discussed above, and prompted a further RAND panel which was also stimulated and enriched by the two Journal of Crohn’s Colitis publications cited above [1, 2]. This further RAND panel, also published in Journal of Crohn’s and Colitis [7], went further in supporting the use of thromboprophylaxis in paediatric IBD and proposed that it should be considered in three distinct groups: all patients with Acute Severe Colitis; all post-pubescent Ulcerative Colitis patients requiring admission for flare and all pre-pubescent Ulcerative Colitis patients with ≥1 risk factor; and all Crohn’s Disease patients requiring admission for flare with ≥1 risk factor.
R Hansen, S Meade, F Torrente, J Kammermeier, N M Croft, L de Ridder, D C Wilson, R Klomberg, D Turner, J Martín-de-Carpi, J Bronsky, E Benchimol, J Amil-Dias, D R Mack, G Walker, M Powar, N Burgess, C H van Ommen, P M Irving, M Samaan, P590 Thromboprophylaxis use in paediatric inflammatory bowel disease: an international RAND appropriateness panel, Journal of Crohn's and Colitis, Volume 16, Issue Supplement_1, January 2022, Pages i526–i527, https://doi.org/10.1093/ecco-jcc/jjab232.716
It is anticipated that the recent RAND panel proposals will be adopted in the next iteration of paediatric IBD guidelines and from there be widely adopted in clinical practice, but it will be some time before the clinical impact of these changes is seen. We can only hope that the rate and severity of this avoidable but potentially catastrophic complication have already peaked, and that in the future we will increasingly see venous thrombosis in paediatric IBD as a rarity.
References
- Kuenzig ME, Bitton A, Carroll MW, et al. Inflammatory bowel disease increases the risk of venous thromboembolism in children: a population-based matched cohort study. J Crohns Colitis. 2021;15:2031–40.
- Aardoom MA, Klomberg RC, Kemos P, et al. The incidence and characteristics of venous thromboembolisms in paediatric-onset inflammatory bowel disease; a prospective international cohort study based on the PIBD-SETQuality Safety Registry. J Crohns Colitis. 2022;16:695–707.
- Kappelman MD, Horvath-Puho E, Sandler RS, et al. Thromboembolic risk among Danish children and adults with inflammatory bowel diseases: A population-based nationwide study. Gut. 2011;60:937–43.
- Turner D, Ruemmele FM, Orlanski-Meyer E, et al. Management of paediatric ulcerative colitis, part 2: Acute severe colitis - An evidence-based consensus guideline from the European Crohn’s and Colitis Organisation and the European Society of Paediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2018;67:292–310.
- Din S, Kent A, Pollok RC, et al. Adaptations to the British Society of Gastroenterology guidelines on the management of acute severe UC in the context of the COVID-19 pandemic: A RAND appropriateness panel. Gut. 2020;69:1769–77.
- Hansen R, Meade S, Beattie RM, et al. Adaptations to the current ECCO/ESPGHAN guidelines on the management of paediatric acute severe colitis in the context of the COVID-19 pandemic: A RAND appropriateness panel. Gut. 2021;70:1044–52.
- Torrente F, Meade S, Benchimol EI, et al. Thromboprophylaxis use in paediatric inflammatory bowel disease: an international RAND appropriateness panel. J Crohns Colitis. 2022 May 24; doi: 10.1093/ecco-jcc/jjac073. Online ahead of print.


