Dan Turner
© Dan Turner
|
Academia can generate high-quality paediatric data during off-label use of drugs: the example of the prospective multicentre VEDOKIDS study
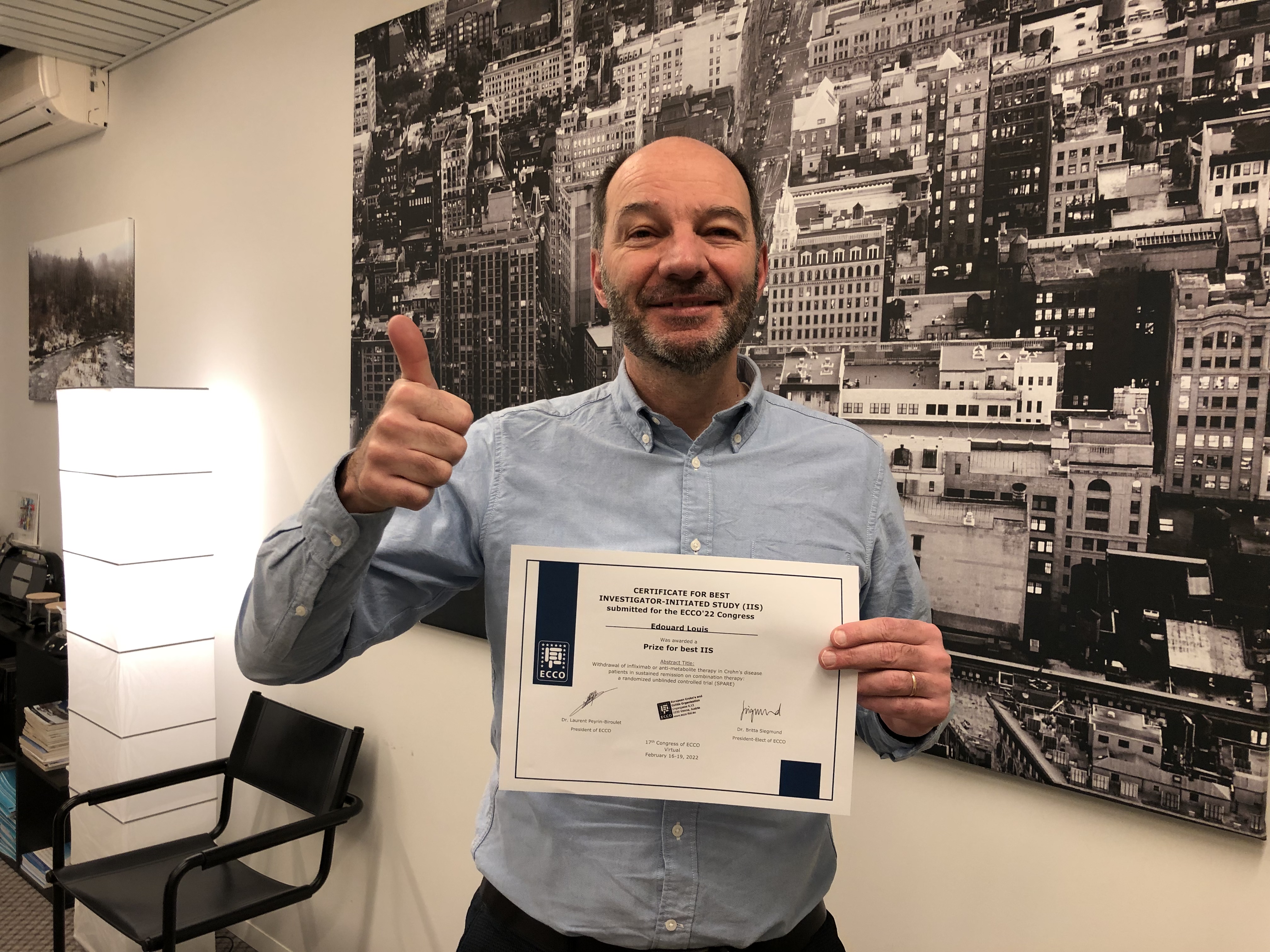
Remarkably, of the numerous biologics approved in adults with IBD, only infliximab and adalimumab have been approved in children. The long delay between approval of new drugs in adults versus children leads to their extensive off-label use, in the absence of appropriate dosing and safety data. Prospective paediatric data regarding vedolizumab are limited to a small phase 2 study (n=88; HUBBLE trial) focusing on pharmacokinetics. A paediatric phase 3 trial is underway but its completion is long overdue, also since vedolizumab is easily accessible in most countries without the constraints of study protocols. With that challenge in mind, once vedolizumab received approval in adults we initiated a prospective cohort study to explore the effectiveness, dosing and safety of vedolizumab in children. The VEDOKIDS study was sponsored by ECCO, The Paediatric Porto group of ESPGHAN and Takeda. Explicit demographic, clinical and safety data were prospectively recorded, and serum was collected for drug levels and stool for faecal calprotectin.















 Eytan Wine
Eytan Wine Wladzia Czuber-Dochan
Wladzia Czuber-Dochan 
 Michel Adamina
Michel Adamina Javier Gisbert
Javier Gisbert

 Pascal Juillerat
Pascal Juillerat